Pegylated Interferon-Based versus Direct-Acting Antiviral-Based Preemptive Treatment of HCV After Adult Living Donor Liver Transplantation
Jae Hyun Kwon1, Gi-Won Song1, Shin Hwang1, Ki-Hun Kim1, Chul-Soo Ahn1, Deok-Bog Moon1, Tae-Yong Ha1, Dong-Hwan Jung1, Gil-Chun Park1, Yongkyu Chung1, Sumin Ha1, Sang-Hyun Kang1.
1Division of Liver Transplantation and Hepatobiliary Surgery, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
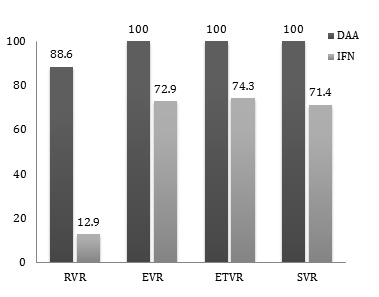 Recurrence of hepatitis C virus (HCV) after liver transplantation is universal. Since the introduction of direct-acting antiviral agent (DAA), treatment for HCV infection has been changed considerably. However optimal treatment for HCV recurrence after liver transplant has not yet been established. We retrospectively evaluated the efficacy DAAs as a preemptive treatment for recurrent HCV infection after living donor liver transplantation (LDLT). From January 2010 to December 2016, total of 105 patients received living donor liver transplantation followed by either pegylated interferon (PegIFN) or DAA-based regimen due to recurrent HCV. All antiviral treatments were started preemptively. Seventy patients were treated with PegIFN and thirty-five patients received DAA after LDLT. Genotype 1b was the most common type (61.9%), followed by 2a (27.6%). In DAA group, 22 recipients were treated with ledipasvir/sofosbuvir, 9 patients received daclatasvir combined with asunaprevir, 3 patients were treated with sofosbuvir, and one patient received sofosbuvir combined with daclatasvir. All thirty-five patients (100%) in DAA group achieved sustained virologic response (SVR), which was significantly higher than fifty recipients (71.4%) in PegIFN group (p<0.001). Recipients in DAA group also showed significantly higher early virologic response (EVR) and end-of-treatment virologic response (ETVR) rate. In PegIFN group, 1-, 3-, and 5-year graft survival after LDLT was 85.7%, 73.9% and 70.7%, respectively. Recipients in DAA group showed 1-, 3-, and 5-year graft survival rate of 100%, significantly higher when compared to PegIFN group (p=0.008). In conclusion, DAA-based treatment for HCV recurrence after LDLT showed effectiveness in achieving SVR and demonstrated better graft survival than PegIFN-based treatment.
Recurrence of hepatitis C virus (HCV) after liver transplantation is universal. Since the introduction of direct-acting antiviral agent (DAA), treatment for HCV infection has been changed considerably. However optimal treatment for HCV recurrence after liver transplant has not yet been established. We retrospectively evaluated the efficacy DAAs as a preemptive treatment for recurrent HCV infection after living donor liver transplantation (LDLT). From January 2010 to December 2016, total of 105 patients received living donor liver transplantation followed by either pegylated interferon (PegIFN) or DAA-based regimen due to recurrent HCV. All antiviral treatments were started preemptively. Seventy patients were treated with PegIFN and thirty-five patients received DAA after LDLT. Genotype 1b was the most common type (61.9%), followed by 2a (27.6%). In DAA group, 22 recipients were treated with ledipasvir/sofosbuvir, 9 patients received daclatasvir combined with asunaprevir, 3 patients were treated with sofosbuvir, and one patient received sofosbuvir combined with daclatasvir. All thirty-five patients (100%) in DAA group achieved sustained virologic response (SVR), which was significantly higher than fifty recipients (71.4%) in PegIFN group (p<0.001). Recipients in DAA group also showed significantly higher early virologic response (EVR) and end-of-treatment virologic response (ETVR) rate. In PegIFN group, 1-, 3-, and 5-year graft survival after LDLT was 85.7%, 73.9% and 70.7%, respectively. Recipients in DAA group showed 1-, 3-, and 5-year graft survival rate of 100%, significantly higher when compared to PegIFN group (p=0.008). In conclusion, DAA-based treatment for HCV recurrence after LDLT showed effectiveness in achieving SVR and demonstrated better graft survival than PegIFN-based treatment.
