A Simple Strategy for Diagnosis of PTDM in Stable Kidney Transplanted Patients
Amin Ussif Dr1, Anders Åsberg prof1,3,5, Thea Anine Strøm Halden Phd1, Espen Nordheim dr1,2, Hallvard Holdaas dr1, Anders Hartmann prof1,2, Trond G Jenssen prof1,4.
1Transplantation Medicine, Oslo University Hospital, Rikshospitalet, Oslo, Norway; 2Institute for Clinical Medicine , University of Oslo, Oslo, Norway; 3School of Pharmacy, University of Oslo, Oslo, Norway; 4Metabolic and Renal Research Group, University of Tromsoe, Tromsoe, Norway; 5Norwegian Renal Registry, Oslo University Hospital, Rikshospitalet, Oslo, Norway
Introduction: The introduction of HbA1c > 6.5% as a diagnostic for diabetes has been challenged for PTDM patients. With this cut-off value the sensitivity has been reported as low as 50% for a PTDM diagnosis in this population in an early phase after transplantation. We aimed to study the utility of fasting plasma glucose fPG together with HbA1c to diagnose PTDM in stable kidney transplanted patients.
Patients and Methods: Altogether 494 non-diabetes transplant recipients underwent an oral glucose tolerance test one year after transplantation in the National Transplantation Center at Rikshospitalet from 2009-2015. Data were retrieved from the biobank and all patients gave written informed consent for use of their data.
Results: Altogether 51 patients (10,3%) had PTDM by the glucose criteria, obtained by fasting glucose at or > 7.0 mmol/l in 38 out of 51 patients (74%). The remaining 13 was diagnosed by 2-hour glucose at or >11.1mmol/l only. The figure shows that 9 of those 13 who did not have elevated fasting plama glucose could be detected by HbA1c elevated at or >6,2%, and 6 was detected by a cut-off at 6,5%. However with 6,2% for cut-off the specificity is reduced and more patients have an erronous PTDM diagnosis according to the OGGT criteria.
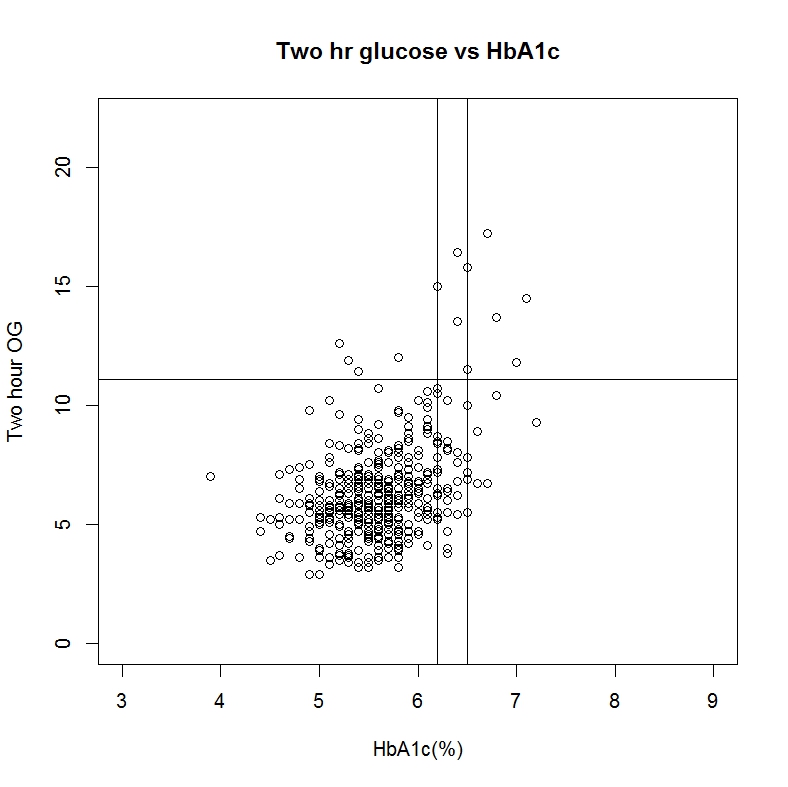 Seven out of 13 patients remained undiagnosed Using HbA1c at or >6,5% as PTDM criterion and 4 of 13 using 6,2%. These 4 patients were followed up for another year and then had regressed to normal fasting plasma glucose and HbA1c values (<6).
Seven out of 13 patients remained undiagnosed Using HbA1c at or >6,5% as PTDM criterion and 4 of 13 using 6,2%. These 4 patients were followed up for another year and then had regressed to normal fasting plasma glucose and HbA1c values (<6).
Discussion: Using standard fasting glucose criteria for diagnosing PTDM patients and add HbA1c criteria on the other patients almost all PTDM caese are captured without an OGGT using a cut-off at 6,2%. With this approach no significant clinical case was missed as these patients had normal glucose one year later. On the other hand many patients are labbelled with PTDM without reaching the OGGT criteria. This may not be a challenge since they will not need drugs or particular counselling beyond normal practice. Using the traditional cut-off of 6,5% some PTDM patients are missed but the specificity obviously is higher.
Conclusion: Although an OGGT is important for diagnosis of prediabetes it appears that a strategy using fasting plasma glucose plus HbA1c criteria will suffice for diagnosis of PTDM in most cases in stable kidney transplant pasients and in particular with a cut-off value of Hba1c of 6,5%.
