Post-transplant Survival in Type 1 Diabetics in Australia and New Zealand
James Hedley1, Patrick J Kelly1, Angela C Webster1,2.
1Sydney School of Public Health, University of Sydney, Sydney, Australia; 2Centre for Transplant and Renal Research, Westmead Hospital, Sydney, Australia
On behalf of the Australian and New Zealand Islet and Pancreas Transplant Registry and contributors.
Introduction: Any advantages of simultaneous pancreas kidney (SPK) transplant over kidney transplant alone (KTA), or pancreas after kidney transplant (PAK) for type 1 diabetics are not well elucidated. We analysed data from the Australian and New Zealand Pancreas and Islet Transplant Registry (ANZIPTR) as well as the Australian and New Zealand Dialysis and Transplant Registry (ANZDATA) to estimate differences in transplant and patient survival by transplant type among recipients with type 1 diabetes.
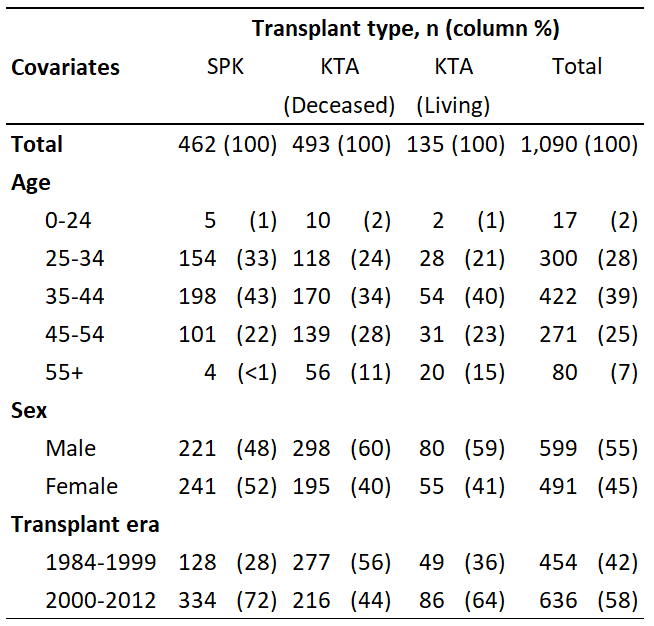
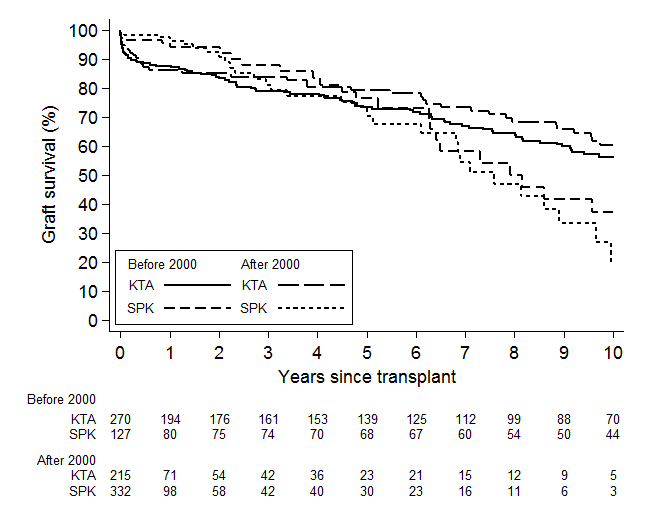
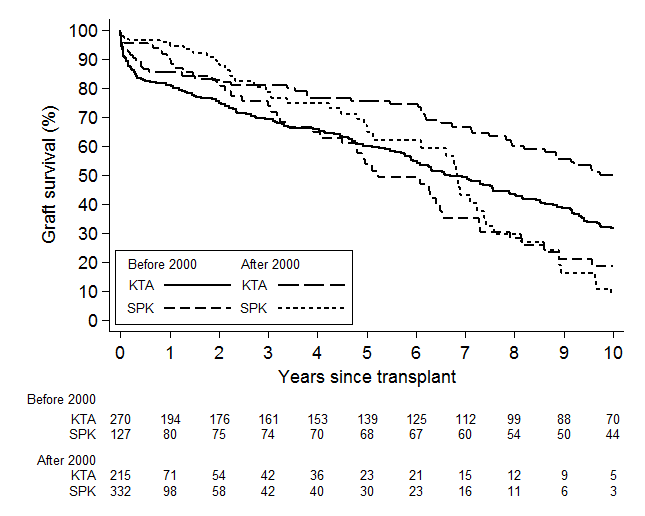
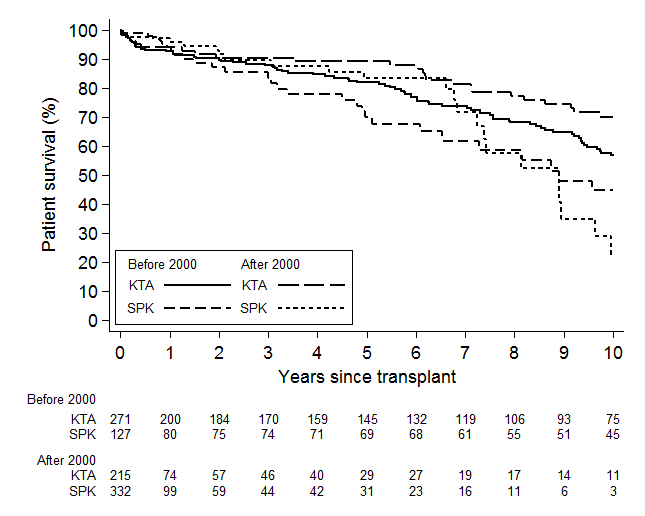
Methods: We conducted an inception cohort study from 1984-2012, using data linkage of ANZIPTR and ANZDATA. We compared kidney graft and patient survival from the date of transplant for SPK and deceased-donor KTA recipients using Cox regression, and censored patients at last known follow-up. We adjusted for age, sex, state/country, previous transplants, age difference between recipient and donor, and immunosuppression used. To meet the proportional hazards assumption we stratified by era (1984-1999, 2000-2012). Kidney transplant failure was analysed including death and censored for death. We also performed secondary analyses comparing SPK transplant to any kidney (living or deceased donor) transplant. Results were hazard ratios (HR) with 95% confidence intervals (CI)
Results: We included 1,090 transplant recipients (462 SPK, 493 deceased donor kidney, 135 living donor kidney). SPK had improved kidney survival compared to deceased donor KTA; including death with function (graft loss HR 0.35; 95% CI 0.21-0.57; p<0.001) and censored for death (graft loss HR 0.45; 95% CI 0.22-0.90; p=0.02). Patient survival was also better among SPK recipients compared to deceased donor KTA (death HR 0.48; 95% CI 0.24-0.95; p=0.03). We found similar results when including living donor KTA prior to 2000 (graft loss including death HR=0.40, censored for death HR=0.56; death HR=0.44). There was some evidence that differences between SPK and all KTA recipients were smaller after 2000 (graft loss including death HR=0.89, censored for death HR=0.55, death HR=0.63).
Conclusion: Overall, patient and kidney transplant survival has improved over time for SPK and KTA recipients. At 5 years, current survival is >90%, and kidney transplant survival >80%. The diminishing advantage of SPK over KTA may reflect selection bias compared to earlier years when SPK donors were scarcer and PAK was more common. Future work will clarify the impact of pancreas transplant function on patient survival, and cause of death.
Australian and New Zealand Pancreas and Islet Transplant Registry . Australian and New Zealand Dialysis and Transplant Registry.
