Revascularization Techniques in Liver Transplantation for Portal Vein Thrombosis and Stenosis: Single Center Experience
Aliaksei Shcherba1, Dzmitry Fedaruk1, Denis Efimov1, Aliaksei Fedaruk1, Siargei Korotkov1, Aleksandr Dzyadzko1, Maksim Katsin1, Andrei Minou1, Oleg Rummo1.
1RSP Center for Organ and Tissue Transplantation, Minsk, Belarus
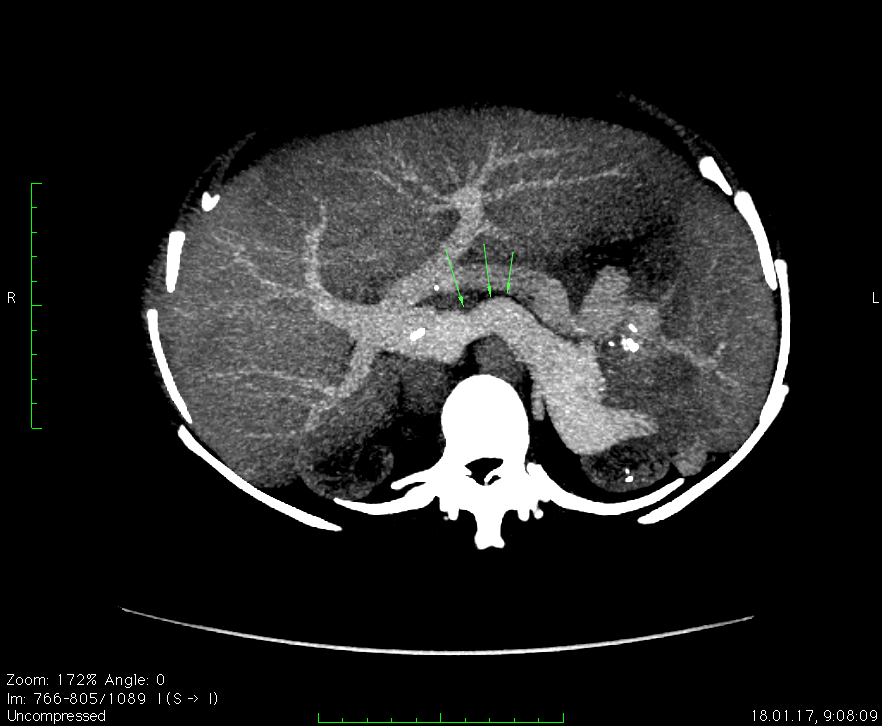
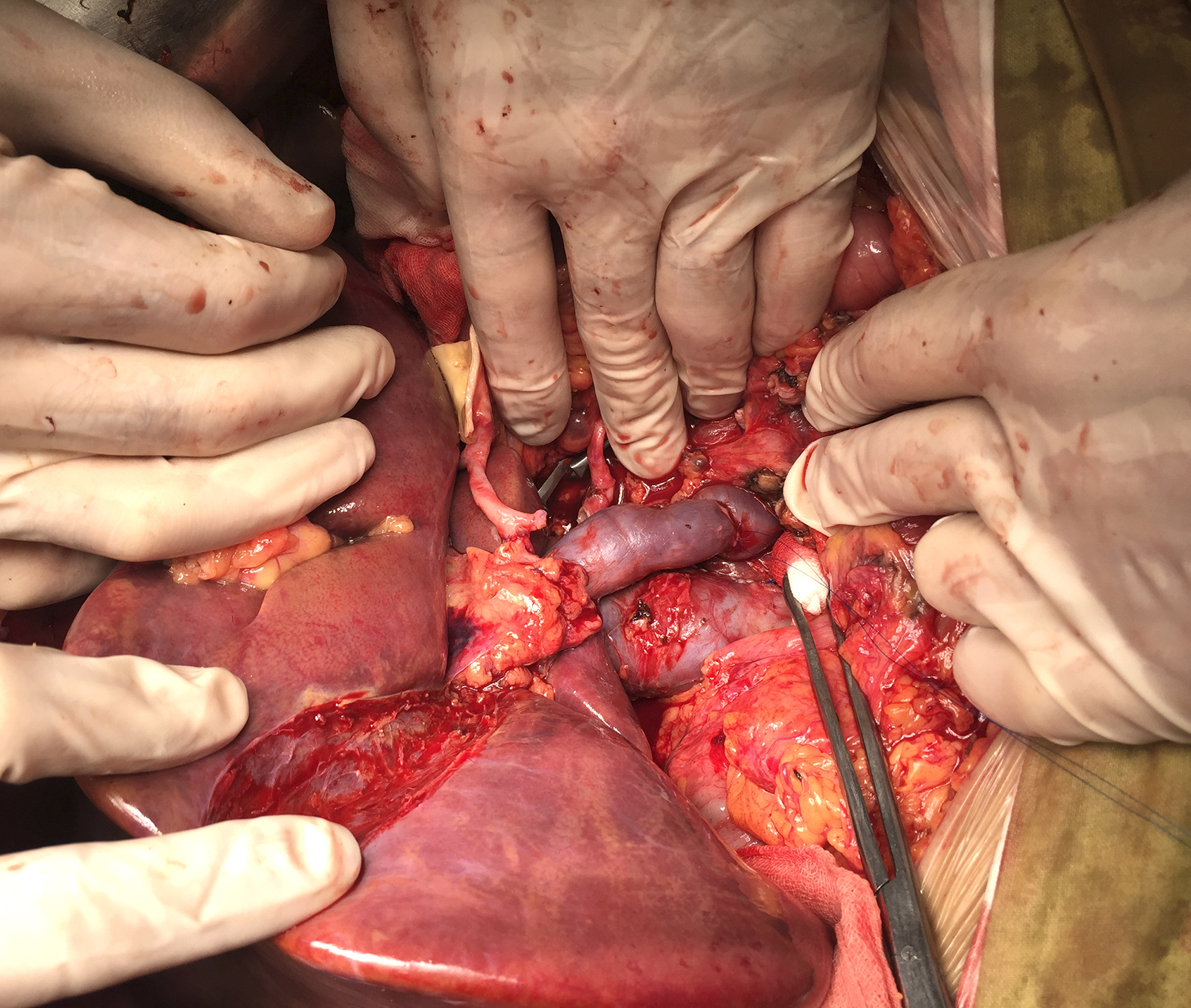
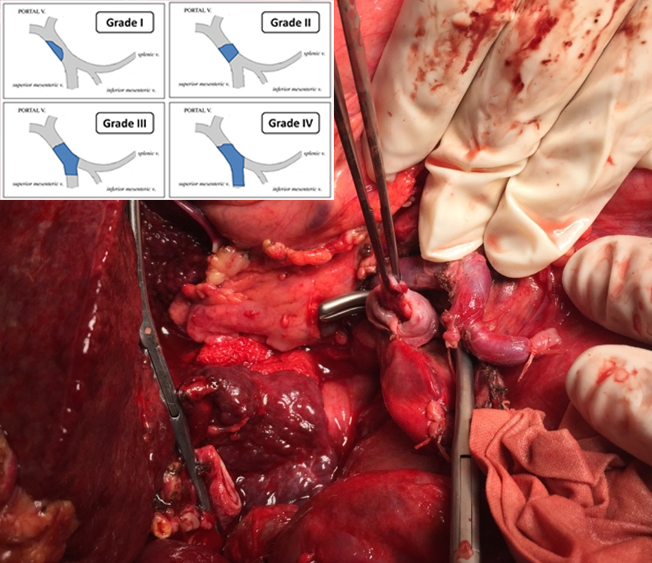
Background:Liver transplantation is the only option for treatment of end-stage liver disease. Portal vein thrombosis (PVT) is a well-recognized complication of liver cirrhosis with reported incidence up to 24% - 32%. In patients with cirrhosis without PVT entering the LT waiting list, the 1-year reported de novo PVT is 7.4-8.4%. However, the incidence of LT performed in PVT patients ranges from 1.2% to 6.6%. The real impact of PVT on post-operative evolution is still under debate. Several approaches were proposed for LT in patients with PV thrombosis or stenosis: thrombectomy and eversion technique, vein transposition (reno-portal, cava-portal), interposition and jump graft, venoplasty and modification for atretic PV, shunt-to-portal anastomosis.
Materials and Methods: 508 liver transplantations had been performed in 2008–Nov. 2017. The overall rate of LT for PVT was 6.1% (31/508). 2 groups of patients were formed: group 1- patients with PV reconstruction& thrombectomy and group 2 – patients with standard PV anastomosis. The PV reconstruction technique depended on PVT grade (Yerdel), age, presence of shunts: thrombectomy (14), reno-portal transposition (5), jump- and interposition graft (1) - adults; cava-portal transposition (6), shunt-to-portal anastomosis (1), confluent-portal (2), venoplasty (2) – pediatric patients.
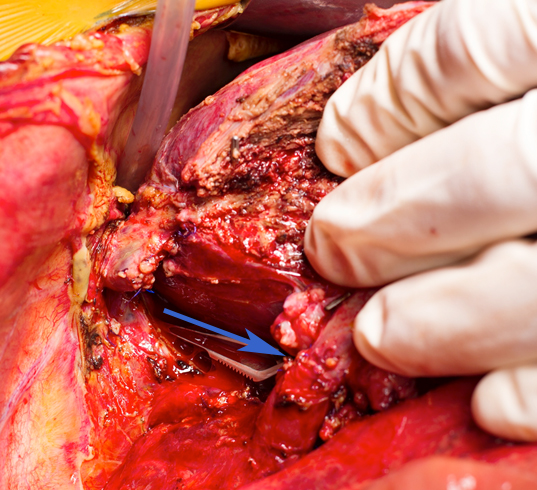
Results: In PV reconstruction& thrombectomy group in adults median age was 56 vs 50 in group2 (p=0.08); median blood loss was 2000 vs 1200 [700; 1700] (p = 0.06), acute kidney injury occurred in 20% cases in group 1 vs 15,7% in group 2 (p = 0.7). Early allograft dysfunction was identified in 10% cases in group 1 vs 24.5% in group 2 (p = 0.3). Post-LT PV thrombosis occurred in 10% in group 1 vs 0,7% in group2 (p = 0.07). Post-LT PV stenosis was not verified in patient from group 1, while in group 2 its rate was 4.8%. Post-LT PV stenting in groups 1 and 2 was performed in 10% and 1,15% , respectively (p = 0.04). 1-year survival rate was 85% vs 93% (p=0.2), respectively.
In pediatric patients median blood loss didn't differ in bouth groups; intra – and post-LT PV thrombosis occurred in 10% in group 1 vs 11.3% in group2 (p =1). Post-LT PV stenting in groups 1 and 2 was performed in 18% and 13,6% , respectively(p =0.6). Acute kidney injury occurred in 9% cases in group 1 vs 18,2% in group 2 (p =1.0). Early allograft dysfunction was identified in 27.3%cases in group 1 vs 37,2% in group 2 (p =1.0). 1-year survival rate was 90% vs 86.4% (p=0.9), respectively.
Conclusion: PV reconstruction is still demanding procedure in LT and assocciated with higher rate of complications in adults. The results of LT in patients with PVT are comparable to patients without PVT when the procedure is thoroughly planned. The kind of PV reconstruction/thrombectomy must be adapted to the PVT grade, age, and presence of suitable shunts.
