Expedited Evaluation for Liver Transplantation: Does Patient Acuity Influence Processes or Outcomes?
Hillary Braun1, Dieter Adelmann MD2, Anna Mello1, Mehdi Tavakol1, Claus U Niemann MD2, Nancy L Ascher MD, PhD1.
1Surgery, University of California, San Francisco, San Francisco, CA, United States; 2Anesthesia, University of California, San Francisco, San Francisco, United States
At our center, the majority of patients listed for liver transplantation (LT) are referred as outpatients by local and regional hepatologists (traditional). However, an increasingly large number of patients are placed on our waiting list after undergoing expedited workup (expedited), whereby they undergo urgent evaluation in the hospital. The purpose of this study was to compare the outcomes of expedited versus traditional patients and to determine whether there are systematic errors or omissions with expedited evaluation.
All adult patients who underwent LT at our institution between 6/1/2012 and 12/31/2015 were reviewed. Patients were excluded if they received a transplant: 1) from a living donor, 2) as a retransplant, 3) for acute liver failure. We compared demographic data, intraoperative details, and outcomes from expedited versus traditional patients using Wilcoxon Rank Sum tests and Chi Squared tests.
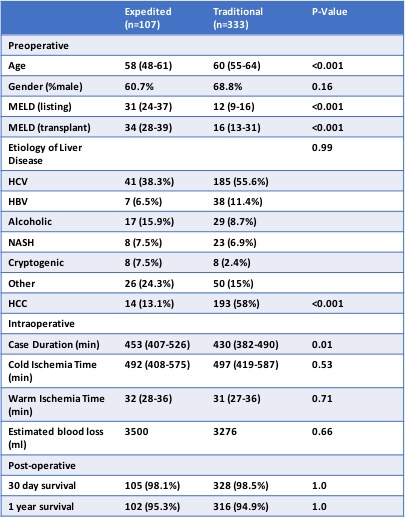
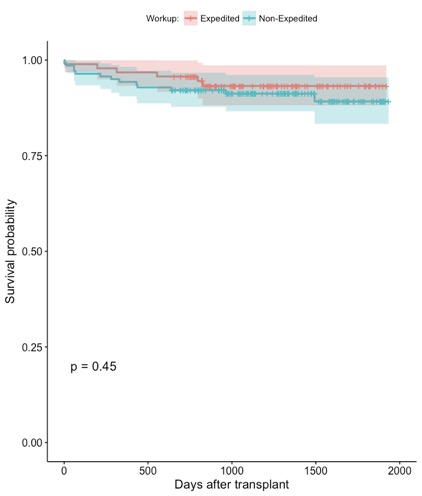
440 patients were included; 107 (24.3%) expedited, 333 (75.7%) traditional. Differences in demographics, intraoperative variables, and post-transplant survival are shown in Figure 1. Expedited patients were significantly younger (58 vs. 60, p<0.001), with greater median MELD at listing and transplant (31 vs. 12, p<0.001; 34 vs. 16, p<0.001, respectively), and longer case duration (453 minutes vs. 430, p=0.01). Between expedited and traditional, there was no significant difference in survival at 30 days (98.1% vs. 98.5%, p=1) or at 1 year (95.3% vs. 94.9%, p=1) post-transplant (Figure 2).
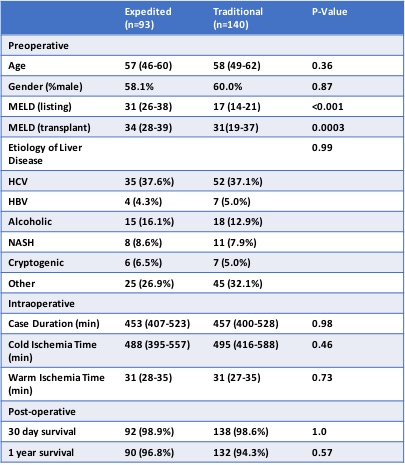
We conducted a subsequent analysis after excluding patients who were transplanted for HCC, which left a cohort of 233 patients, 93 (40%) expedited and 140 (60%) traditional (Figure 3). There was no difference in age (57 vs. 58, p=0.36), gender breakdown (58.1% male vs. 60% male, p=0.87), or most common indication (HCV, 37.6% vs 37.1%). There was also no significant difference in case duration, WIT, CIT, or survival at 30 days and 1 year post-transplant.
Expedited LT evaluation occurs quickly but utilizes inpatient resources. It also impacts decision making during our selection committee meetings, as the acuity of these patients on presentation can be dramatic. In this initial review of our data, we found no significant difference in post-transplant survival for expedited versus traditional patients. However, we suspect that there are significant differences in time to transplant and cost of evaluation for these cohorts. Additionally, and perhaps most importantly, we anticipate that selection committee assessment is influenced by the urgency of these evaluations and may result in risk factors or contraindications being overlooked. Finally, we think there may be a difference in quality of donor organs that these groups receive. We are currently investigating MELD-matched comparisons, analyzing selection committee reports, increasing the granularity of our data collection, and expanding our cohort.