Use of Tissue Plasminogen Activator (tPA) and Histidine-Tryptophan-Ketoglutarate Solution (HTK) in Donation after Circulatory Death (DCD) Liver Transplant Prevents Ischemic Cholangiopathy
Arianna E Cabrales1, Richard S Mangus1, Chandrashekhar A Kubal1.
1Department of Surgery, Transplant Division, Indiana University School of Medicine, Indianapolis, IN, United States
Introduction:The use of liver grafts obtained using a donation after circulatory death (DCD) protocol has not reached its full potential. Many centers have reported inferior outcomes, including lower graft and patient survival, when transplanting these livers. A primary complication is ischemic cholangiopathy (IC), which is associated with graft loss and need for re-transplantation. A theory for this IC is that the blood flow to the biliary system develops thrombi during the warm time of the organ procurement. These thrombi are not fully cleared during graft procurement and transplant, and result in persistent biliary ischemia in the weeks after transplant. We have demonstrated early success in avoiding IC by using a combination of histidine-tryptophan-ketoglutarate solution (HTK) and tissue plasminogen activator (tPA) during procurement. HTK is much less viscous than University of Wisconsin solution (UW), so we feel that HTK provides a better flush of the microvasculature, and the tPA is a thrombolytic which lyses any thrombi which have formed in the arterial capillary system. This paper reports the long term outcomes for combined HTK and tPA use in DCD livers at a single center.
Methods: Records for liver transplants at a single center were reviewed (2001 to 2017). DCD organ procurement was performed according to carefully established protocols. For all patients, there was a 5-minute wait after declaration of cardiac death by an independent physician. After that wait time, the surgeons performed rapid clamping and cannulation of the abdominal aorta. Decompression of the vena cava was generally through the right atrium. The flush included an initial bolus with HTK (1 liter) to clear some of the blood. This bolus was followed by infusion of tPA in 1L NS. After this, the liver was further flushed with HTK until clear (usually 3-4 liters total HTK). Overall volume of solution was less than 5 liters.
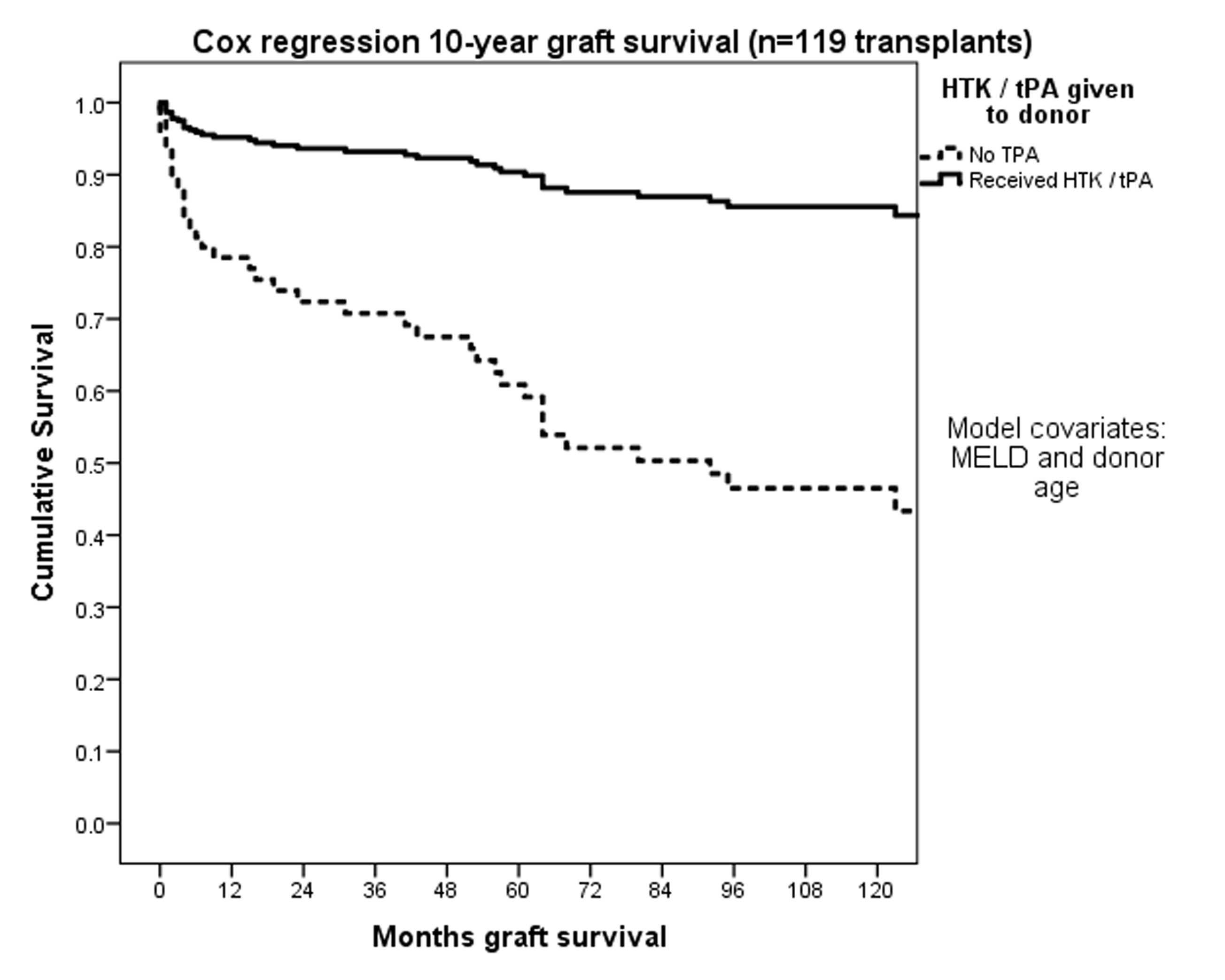
Results: Fifty-seven patients received livers from combined HTK/tPA procurement (48%) and 62 from non-tPA procurements (52%, includes cases with either HTK or UW alone). The HTK/tPA grafts were transplanted into patients who were older and higher MELD scores. The HTK/tPA grafts had less ischemia time (both cold and warm). The liver grafts with HTK/tPA had better survival at 1 week and 3 months (p=0.09, p=0.06) and also after one-year (95% vs 79%, p=0.01). Cox regression survival demonstrated significantly higher survival for HTK/tPA grafts (88% vs 45% at 10-years; p<0.01). There were no cases of IC in the HTK/tPA group. Higher survival rates with the combined HTK and thrombolytic therapy in DCD liver transplantation changed the overall use of DCD livers at this center. We began to use extended criteria DCD grafts from donors that were older (> age 50, heavier (BMI>35), and from other geographic regions. As we increased use of the extended criteria DCDs, there was no change in clinical outcomes with consistently high graft survival.
Conclusions: These results demonstrate that DCD liver donor flush with combined HTK/tPA yields a marked decrease in IC. We experienced no cases of IC when combined HTK/tPA were used. As we experienced these successful outcomes, we were able to expand our use of these grafts to more high risk donors and recipients.
