Beneficial Effect of ABO Incompatibility on De Novo DSA Production after Kidney Transplantation
Takaaki Kobayashi1, Manabu Okada1,5, Kenta Iwasaki2, Kosei Horimi1, Yutaka Matsuoka1, Yuko Miwa2, Kazuharu Uchida3, Asami Takeda4, Norihiko Goto5, Shunji Narumi5, Yoshihiko Watarai5.
1Department of Renal Transplant Surgery, Aichi Medical University School of Medicine, Nagakute, Japan; 2Department of Kidney Disease and Transplant Immunology, Aichi Medical University School of Medicine, Nagakute, Japan; 3Department of Transplant Surgery, Masuko Memorial Hospital, Nagoya, Japan; 4Department of Nephrology , Nagoya Daini Red Cross Hospital, Nagoya, Japan; 5Department of Transplant and Endocrine Surgery, Nagoya Daini Red Cross Hospital, Nagoya, Japan
Introduction De novo donor specific HLA antibodies (DSA)-induced chronic antibody-mediated rejection (ABMR) is one of major obstacles to long term graft survival. Recently, ABO incompatible kidney transplantation (ABO-I) has showed favorable graft survival. We have reported that anti-A/B antibody binding could cause graft accommodation, which demonstrated protective effects against graft injury due to upregulation of complement regulatory proteins (CD55/CD59) and downregulation of HLA class II antigens. The purpose of this study was to elucidate the effect of ABO incompatibility on de novo DSA production after kidney transplantation.
Methods HLA-DRB1/3/4/5 and DQB1 epitope mismatch (MM) levels and de novo DSA production were examined in 681 living donor kidney transplantations [449 ABO-identical/compatible (ABO-Id/C), 232 ABO-I] performed between 2008 and 2015. Desensitization in ABO-I included rituximab (RIT, n=164), splenectomy (SPX, n=10) and neither (NONE, n=58) due to low anti-A/B antibody titers.
Results De novo DSA were detected in 80 recipients (11.7%) including DSA against class I (n=9), class I+DQ (n=2), DR (n=14), DQ (n=50) and DR+DQ (n=5). Biopsy-proven chronic ABMR was significantly associated with DR DSA (HR 14.7, P=0.0003) and DQ DSA (HR 33.1, P<0.0001), but not class I DSA. Therefore, only class II (DR and/or DQ) DSA were considered in this study. Epitope MM levels of DRB1/3/4/5 and DQB1 were significantly correlated with production of DR and DQ DSA, respectively (Fig. 1). De novo DSA free graft survivals with moderate MM levels (6-15 DRB1/3/4/5 MM and 1-5 DQB1 MM) were significantly higher in ABO-I (DR 100%, DQ 100%) than in ABO-Id/C (DR 96.3% P=0.0378, DQ 90.7% P=0.0143) (Fig. 2). ABO-I without rituximab pretreatment also exhibited the favorable results for de novo DSA production (Fig. 3).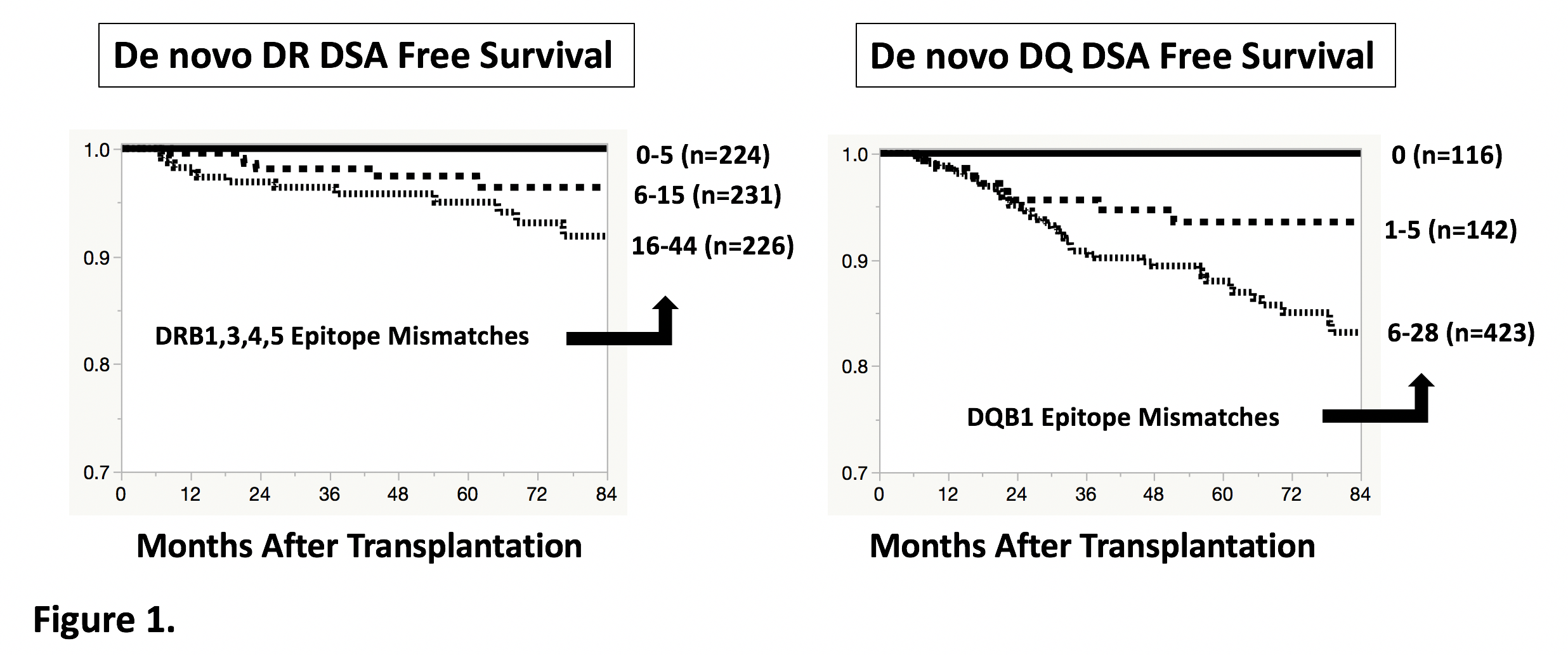
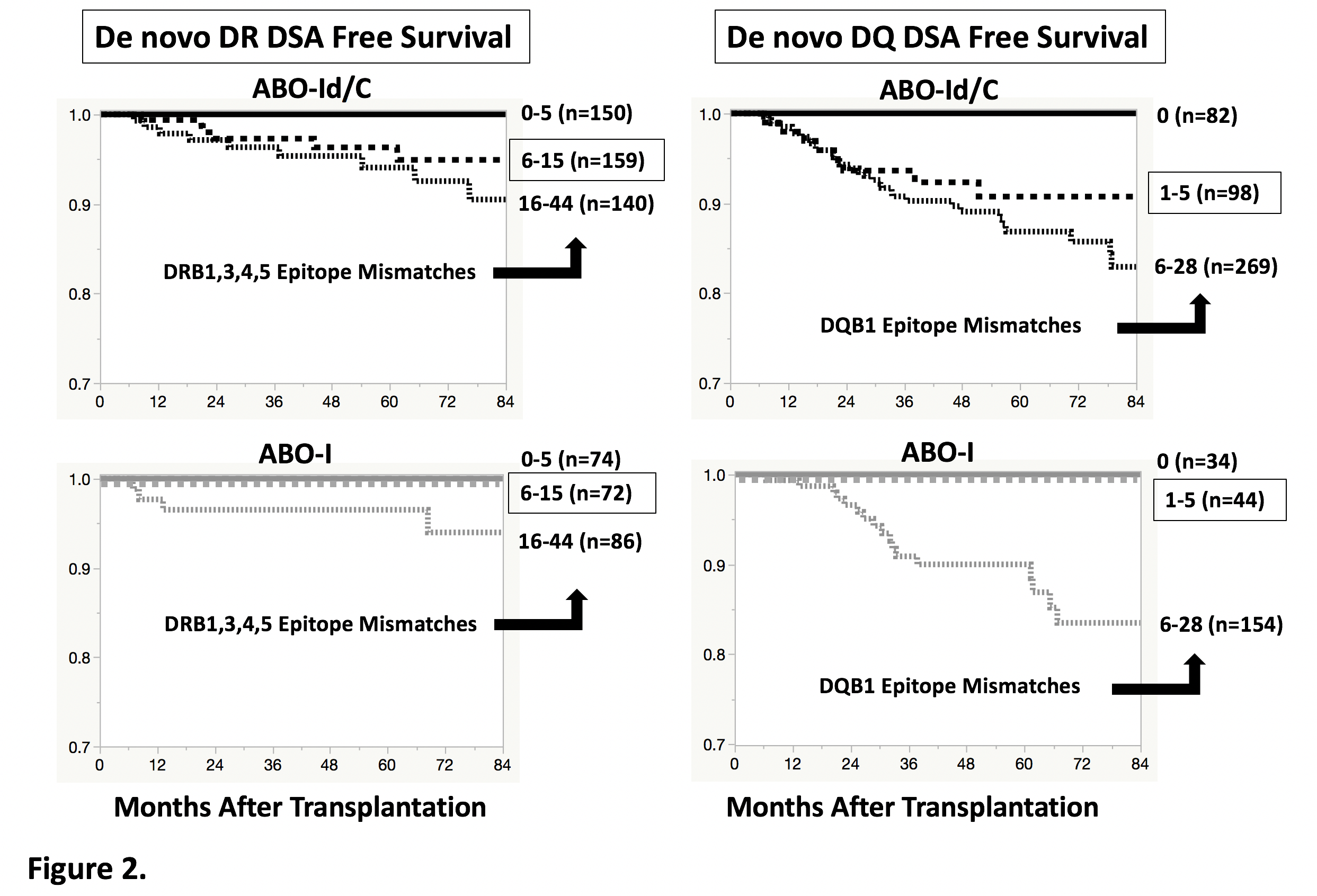
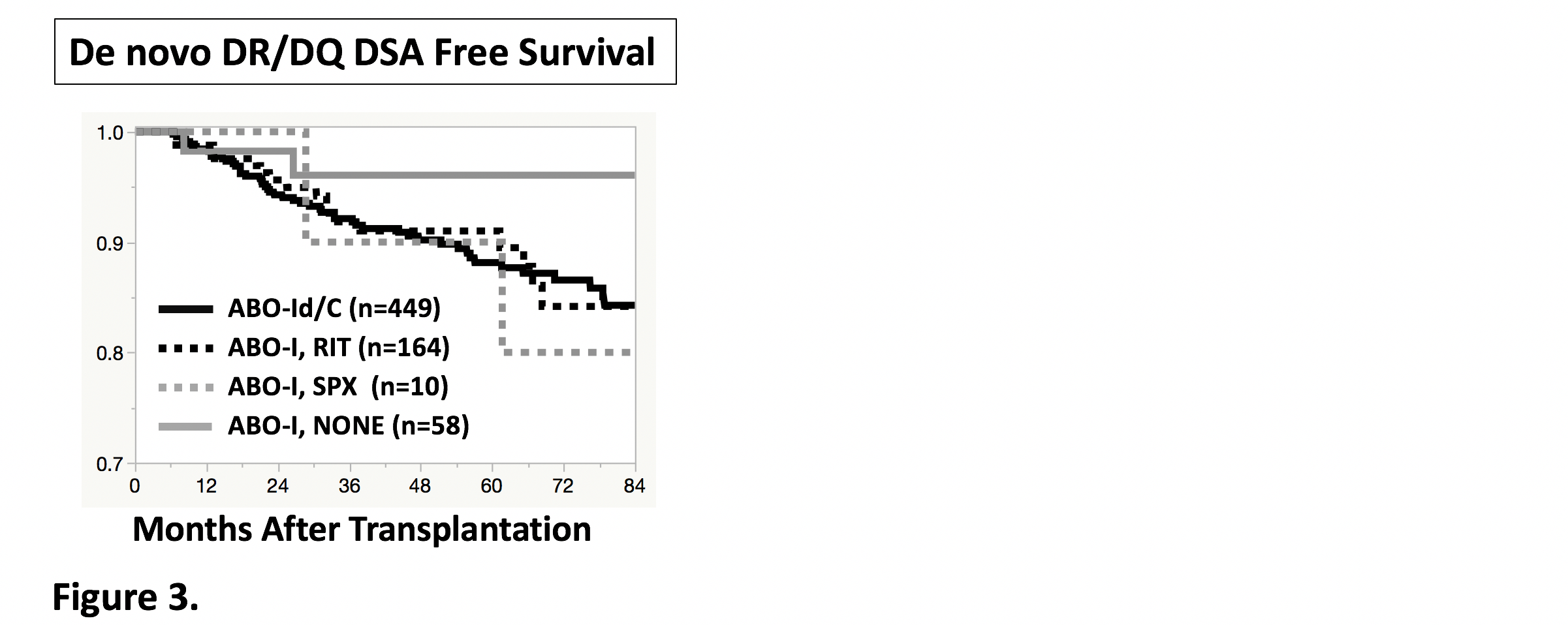
Conclusions DRB1/3/4/5 and DQB1 epitope MM levels could predict the risk of de novo DSA production. Protective effect against de novo DSA production was observed in ABO-I with moderate levels of DRB and DQB epitope MM. Beneficial effect of ABO incompatibility may be elicited by anti-A/B antibody binding to the graft, rather than rituximab pretreatment.
