Pseudocyst of Pancreas Transplant Allograft,a Rare Complication
Jeffrey Stern1, Kunal Yadav1, Renee Cholyway1, Gaurav Gupta2, Adrian Cotterell1, Marlon Levy1.
1Department of Surgery, Virginia Commonwealth University, Richmond, VA, United States; 2Division of Nephrology, Virginia Commonwealth University, Richmond, VA, United States
Background: Simultaneous pancreas and kidney (SPK) transplantation is the treatment of choice for patients with type-1 diabetes mellitus and end stage renal disease. Pancreatic pseudocyst is both a very rare and rarely reported complication after SPK. We report successful management of a patient who developed a pancreatic pseudocyst 15 years after transplantation.
Case Report: A 58 year-old male underwent SPK in 2002. He had enteric drainage initially, but was converted to bladder drainage after developing recurrent psoas abscess and pancreatic fistula. He did well for the next 15 years with good pancreas and renal allograft function, but with repeated episodes of allograft pancreatitis. He presented with pain over the pancreas allograft, serum amylase and lipase elevation consistent with allograft pancreatitis.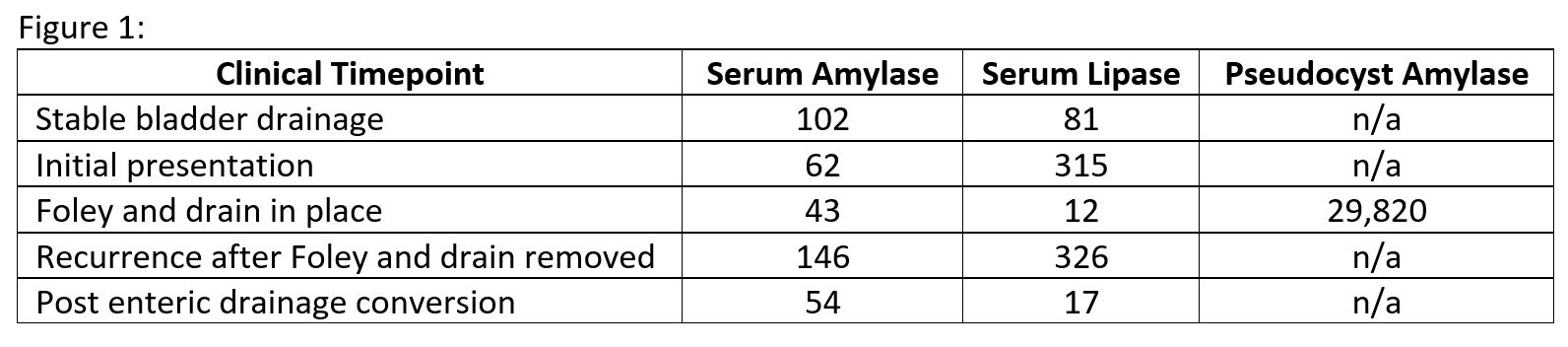 Cross-sectional imaging showed a 6 x 3 x 8 cm cystic fluid collection in the tail of the transplanted pancreas, dilatation of the pancreatic duct and donor duodenum, and marked distention of the urinary bladder with a normal prostate.
Cross-sectional imaging showed a 6 x 3 x 8 cm cystic fluid collection in the tail of the transplanted pancreas, dilatation of the pancreatic duct and donor duodenum, and marked distention of the urinary bladder with a normal prostate.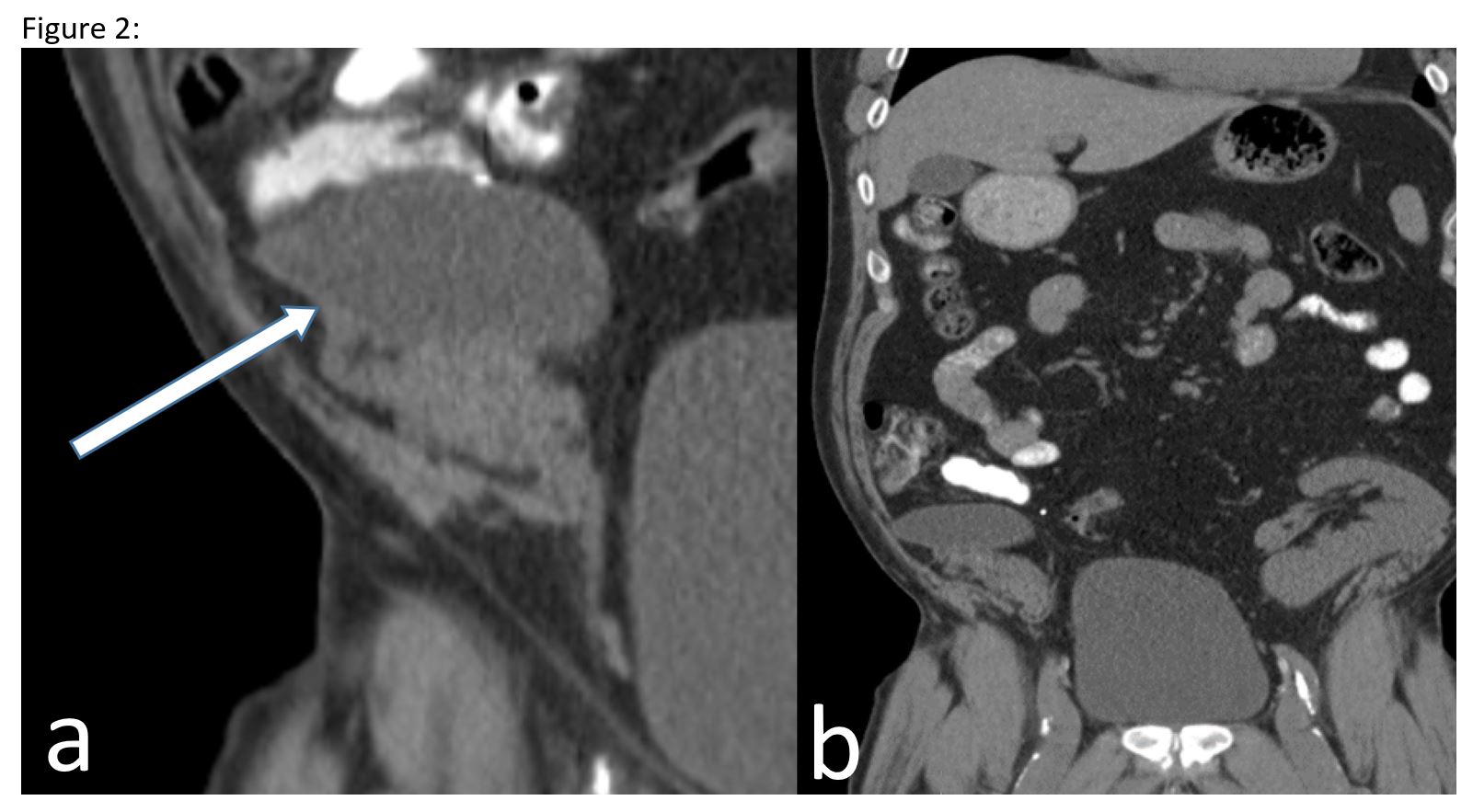 The pancreatic cyst was drained percutaneously and contained high levels of amylase (29,820 units/L) consistent with a pancreatic pseudocyst. A Foley catheter was then placed to decompress the bladder to prevent reflux pancreatitis. Placement of the bladder catheter and the pseudocyst drain resulted in normalization of pancreatic enzymes and symptomatic pain relief. After removal of the drain and the catheter, the pancreatitis and pain recurred. Cross-sectional imaging showed recurrent pancreatic pseudocyst with urinary bladder distention.
The pancreatic cyst was drained percutaneously and contained high levels of amylase (29,820 units/L) consistent with a pancreatic pseudocyst. A Foley catheter was then placed to decompress the bladder to prevent reflux pancreatitis. Placement of the bladder catheter and the pseudocyst drain resulted in normalization of pancreatic enzymes and symptomatic pain relief. After removal of the drain and the catheter, the pancreatitis and pain recurred. Cross-sectional imaging showed recurrent pancreatic pseudocyst with urinary bladder distention.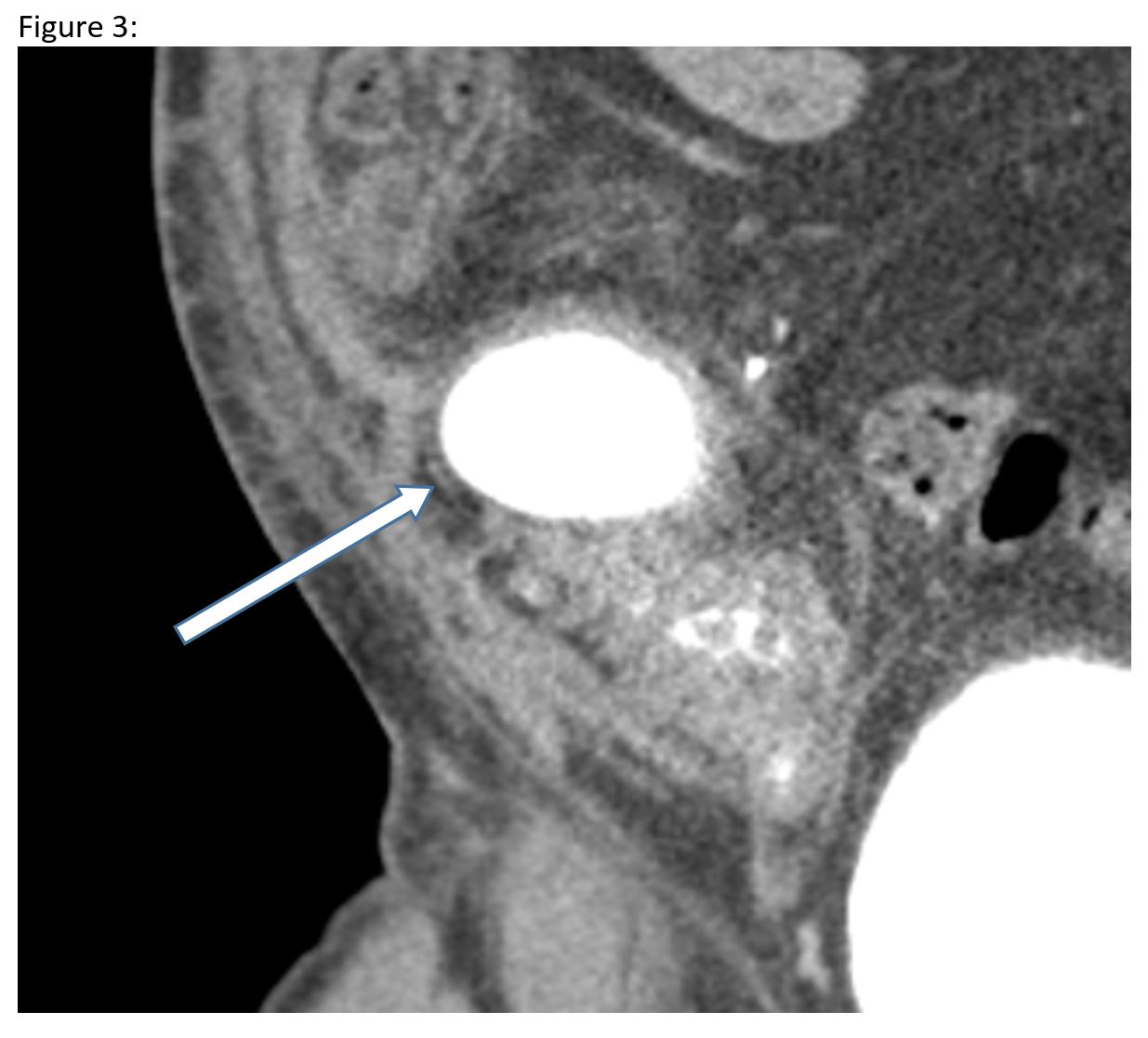 To achieve a more durable solution in the setting of the patient’s persistent urinary retention, he was converted back to enteric drainage. This resulted in normalization of pancreatic enzymes and resolution of the pseudocyst. His post-operative course was prolonged, but a full recovery with maintained pancreas and renal allograft function was achieved.
To achieve a more durable solution in the setting of the patient’s persistent urinary retention, he was converted back to enteric drainage. This resulted in normalization of pancreatic enzymes and resolution of the pseudocyst. His post-operative course was prolonged, but a full recovery with maintained pancreas and renal allograft function was achieved.
Conclusions: In bladder drained pancreatic allografts, urinary retention can result in reflux pancreatitis leading to pseudocyst formation. We describe enteric conversion as a successful management strategy for this rare complication.
