Intestinal Mucosal Barrier Disruption and Microfold Cells Impairment were Required for Invasive Fungal Infection after Living Donor Liver Transplantation.
Jiang Liu1, Xiaobing Liu1, Chungmau Lo1, Kwan Man1.
1Department of Surgery, The University of Hong Kong, Hong Kong, P.R. China
Introduction and Objective: Post-transplant invasive fungal infection (IFI) is a critical problem with high mortality for patients receiving living donor liver transplantation (LDLT), however, the underlying mechanism stays unclear. Hence, identifying the risk factors and understanding the mechanisms of IFIs are essential to improve outcome of LDLT patients.
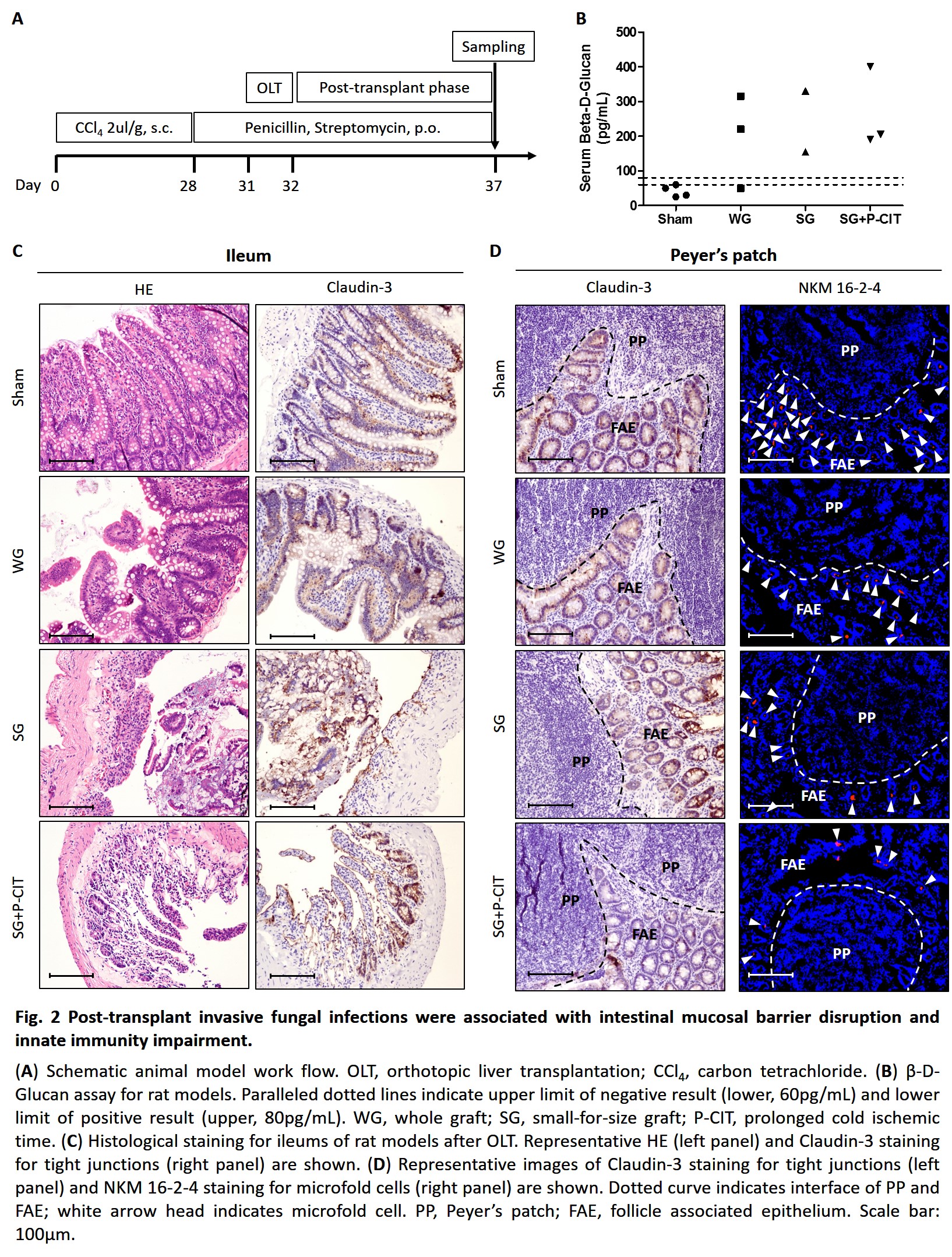
Materials and Methods: Clinical characteristics of patients diagnosed with opportunistic fungal infections compared with non-infected patients after living donor liver transplantation were analyzed in a retrospective cohort from 1994 to 2017. The correlation between marginal graft injury and incidence of IFIs was investigated by 1, 3-β-D-Glucan assay in rat orthotopic liver transplantation models using marginal grafts. And intestinal mucosal structural integrity as well as microfold cells of intestinal Peyer’s patches were also investigated in animal models.
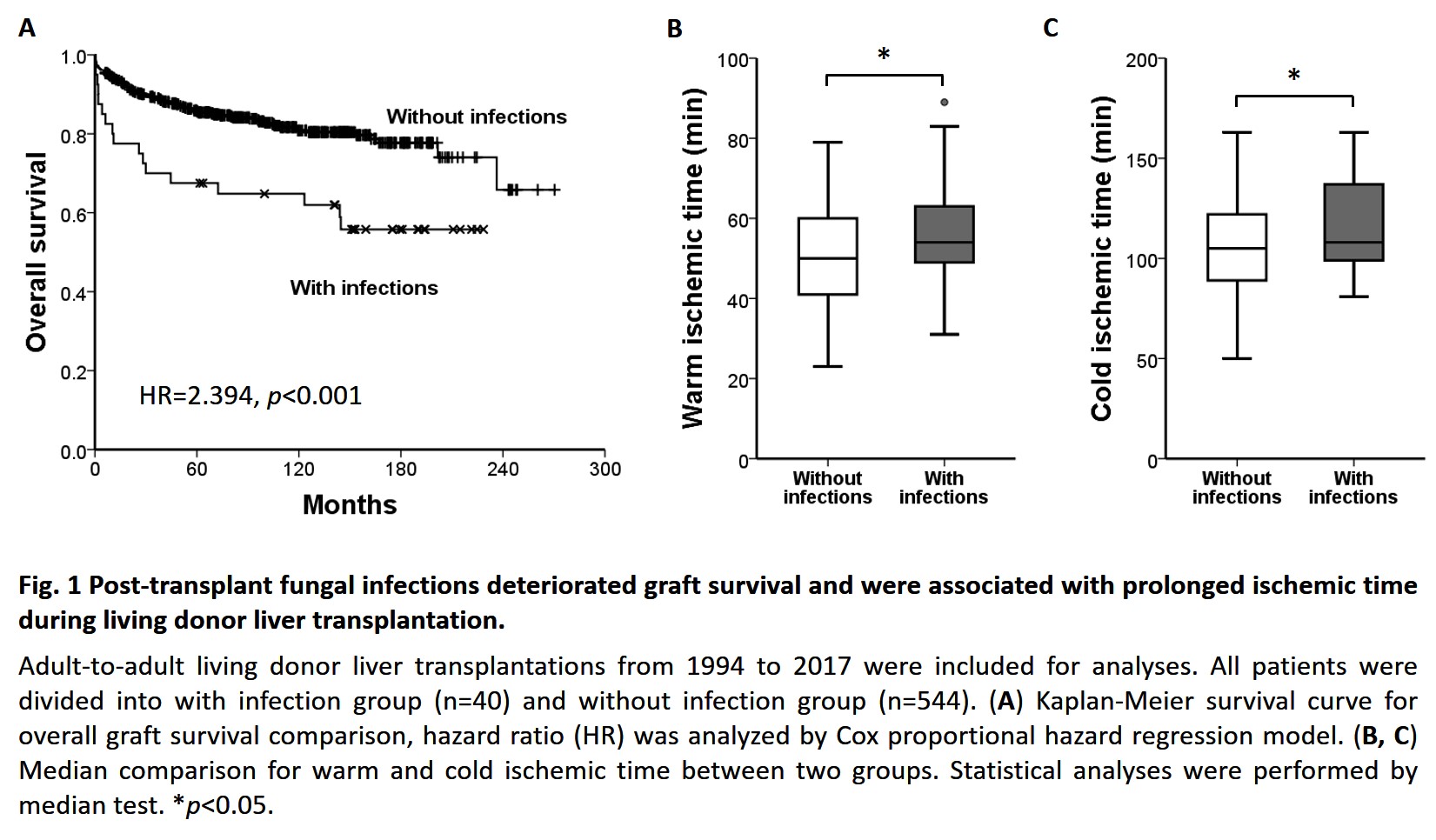
Results and Discussion: 44 out of 584 patients were diagnosed with opportunistic fungal infections after LDLT, and they were presented with higher hospital mortality (15% vs 2.8%, p=0.002) as well as long term graft failure compared with patients without infections (Fig. 1A, HR=2.394, p<0.001). In addition, prolonged cold ischemic time and warm ischemic time were identified associated with post-transplant opportunistic infection occurrence (Fig. 1BC). In rat orthotopic liver transplantation models, incidence of IFIs and median serum β-D-Glucan value were higher in small-for-size graft, as well as in graft with prolonged ischemic time compared to whole-size graft and sham operation groups (Fig. 2AB). Furthermore, disruption of intestinal villi structure and loss of tight junctions were found associated with more severe liver graft injury (Fig. 2C). And damage to tight junctions of intestinal follicle associated epithelium covering Peyer’s patches as well as deletion of functional microfold cells (M cells) were also found in liver graft after transplantation, whilst the situation was even worse after ischemic time was extended (Fig. 2D).
Conclusion:
Small-for-size and ischemic injury of liver graft rendered LDLT patients more vulnerable to gut derived invasive fungal infections by disrupting intestinal mucosal barrier and impairing intestinal innate immunity.
