Patient and Graft Outcome Among High Immunologic Risk Renal Transplant Recipients
Jeffrey Mora1, Concesa B Cabanayan-Casasola2, Florecita R Padua3, Myrna T Mendoza4.
1Adult Nephrology, National Kidney and Transplant Institute, Quezon City, Philippines; 2Adult Nephrology, National Kidney and Transplant Institute, Quezon City, Philippines; 3Immunology, National Kidney and Transplant Institute, Quezon City, Philippines; 4Infectious Disease, National Kidney and Transplant Institute, Quezon City, Philippines
Introduction: Kidney transplantation (KT) is the preferred treatment for ESRD. However, some patients had prior HLA sensitization making them immunologically high risk for graft rejection and poorer graft survival. Hence, desensitization protocols were developed to clear the circulating alloantibody and therefore prevent rejection. However, desensitization therapy is expensive and associated with higher risk of infection.
Our study looked at the patient and graft survival of high immunologic risk KT recipients at National Kidney and Transplant Institute.
Methods: This is a retrospective cohort study that included patients who underwent KT from January 2012 to June 2016. Out of 1,804 patients, 52 were highly sensitized and we divided them into DSA positive and DSA negative group, and further divided into subgroups based on PRA; ≤20%, >20% ≤80%, and >80%.
Results: There were 42.3% DSA(+) and 57.7% DSA(-) patients. Male to female ratio was 1:2. There were 56.8% multigravid, 63.5% had prior blood transfusions.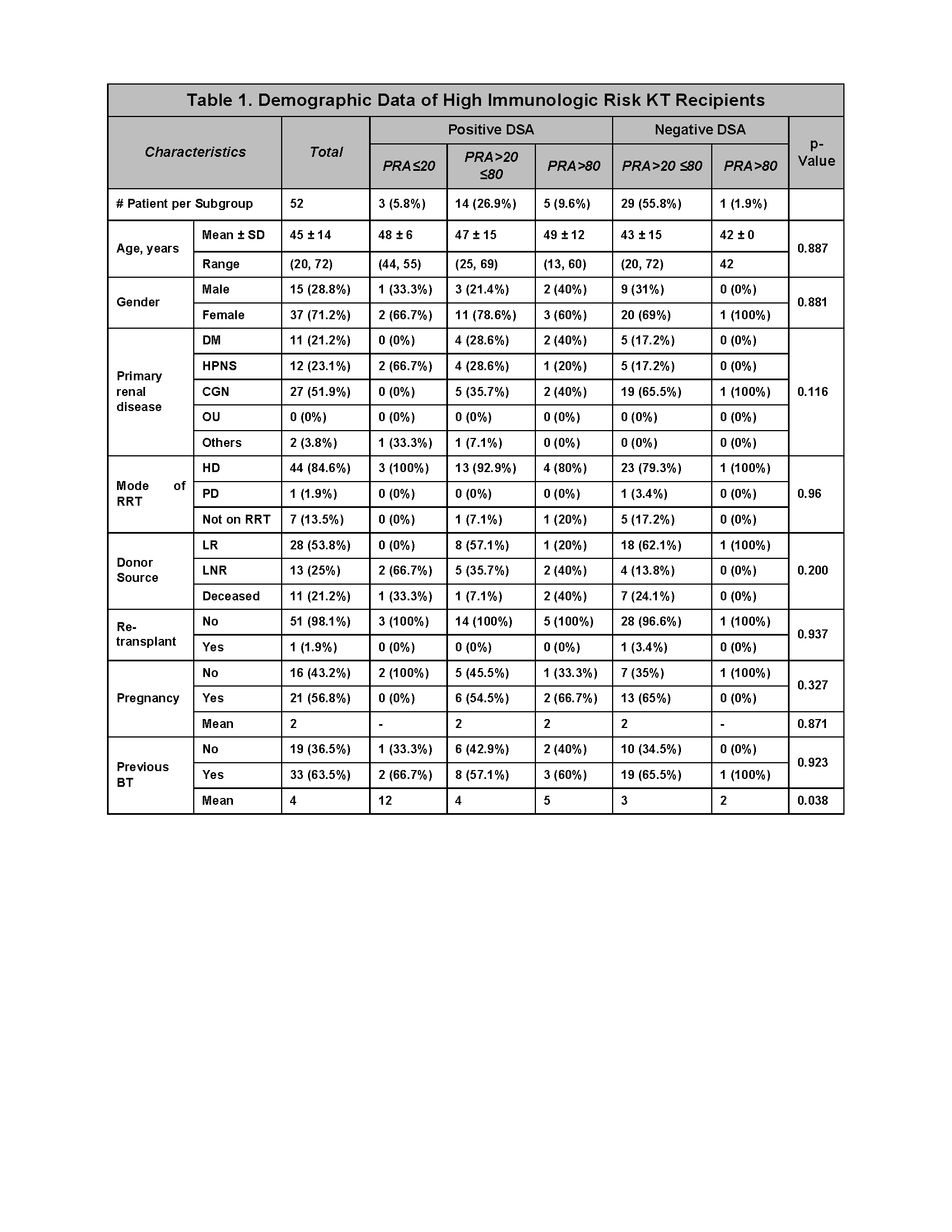 There were 21.2% who underwent desensitization: 9 (81.8%) had Rituximab+Plasmapheresis(TPE)+Intravenous immunoglobulin(IVIg), 1 (9.1%) had TPE+IVIg, and 1 (9.1%) had TPE+Rituximab.
There were 21.2% who underwent desensitization: 9 (81.8%) had Rituximab+Plasmapheresis(TPE)+Intravenous immunoglobulin(IVIg), 1 (9.1%) had TPE+IVIg, and 1 (9.1%) had TPE+Rituximab.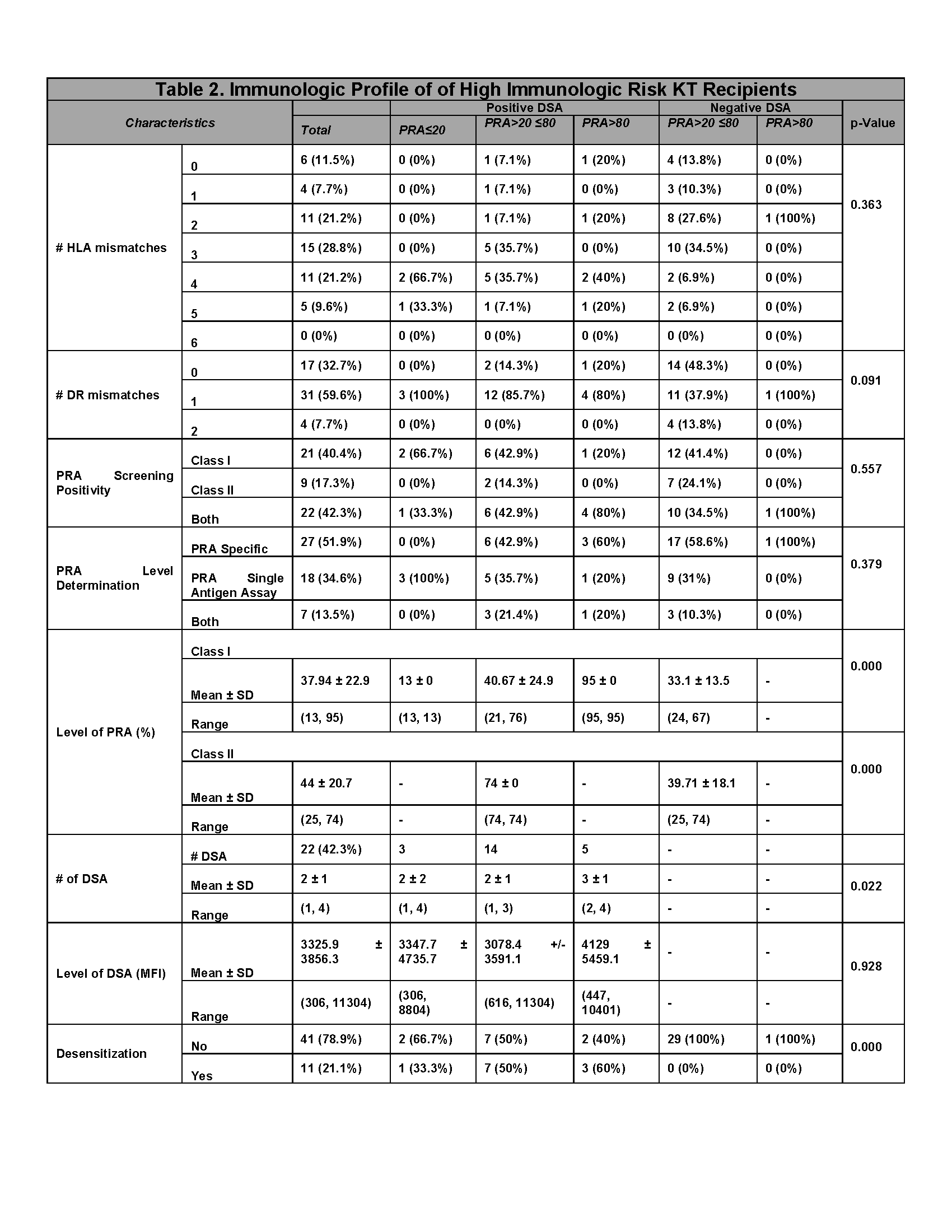
Rabbit ATG was given to 92.3% and 7.7% were given Basiliximab. Three patients (2 DSA(+), 1 DSA(-)) were given Rituximab as induction therapy in addition to rATG.
Most common immunosuppresive was Tacrolimus+Mycophenolic acid, 90.4%. All patients were on Prednisone. The mean Creatinine level (mg/dL) were 1.0, 1.0, 1.3, and 1.0 mg/dL at 6, 12, 24, and 60 months post KT, respectively. The 5-year biopsy-proven acute rejection rate was 9.6% and higher among DSA(+). In contrast, chronic rejection rate was 7.7% and higher among DSA(-). The most common complication was infection (26.9%).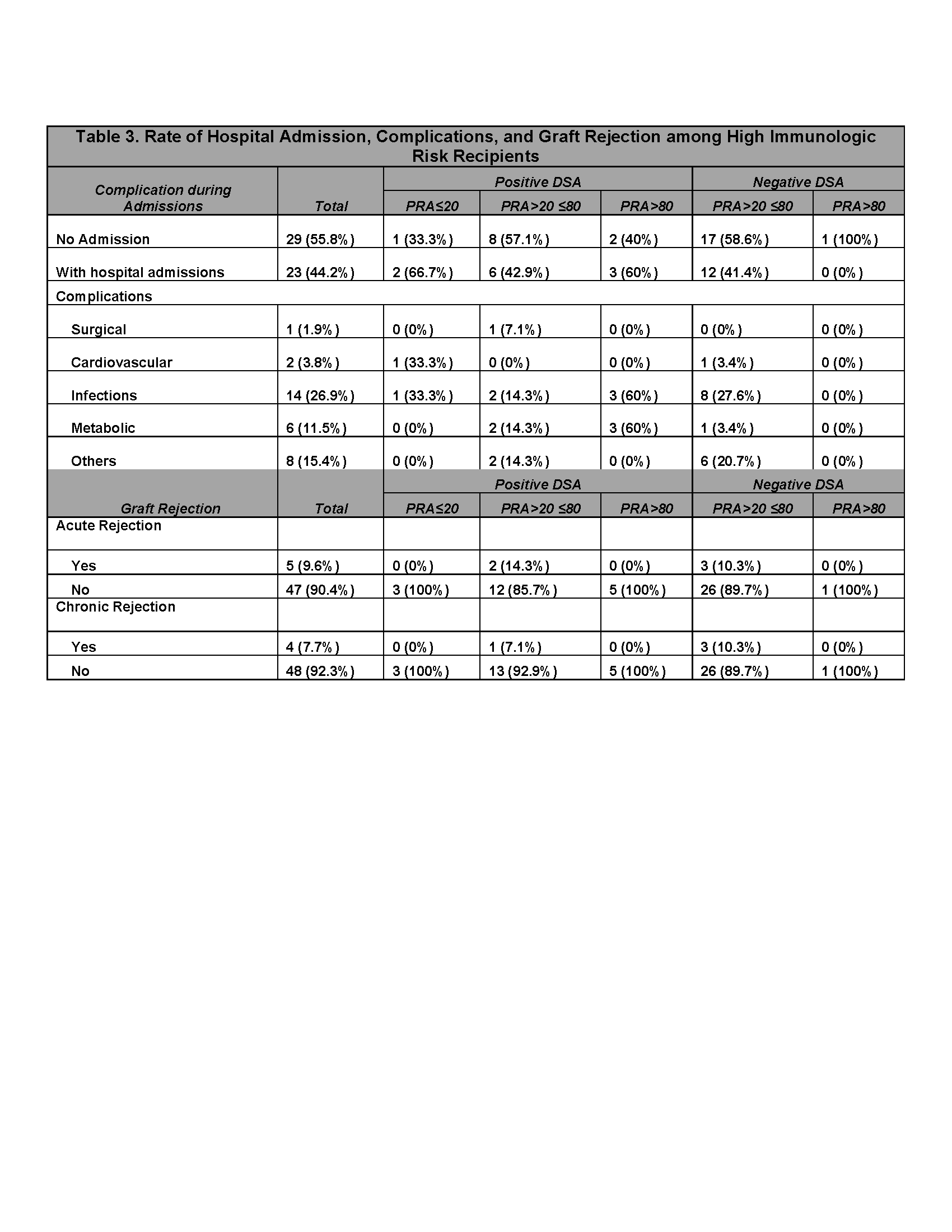
The patient survival was 95, 81, and 80% at 1,2, and 5 years post KT. The graft survival was 95, 75, and 70% at 1,2, and 5 years post KT. 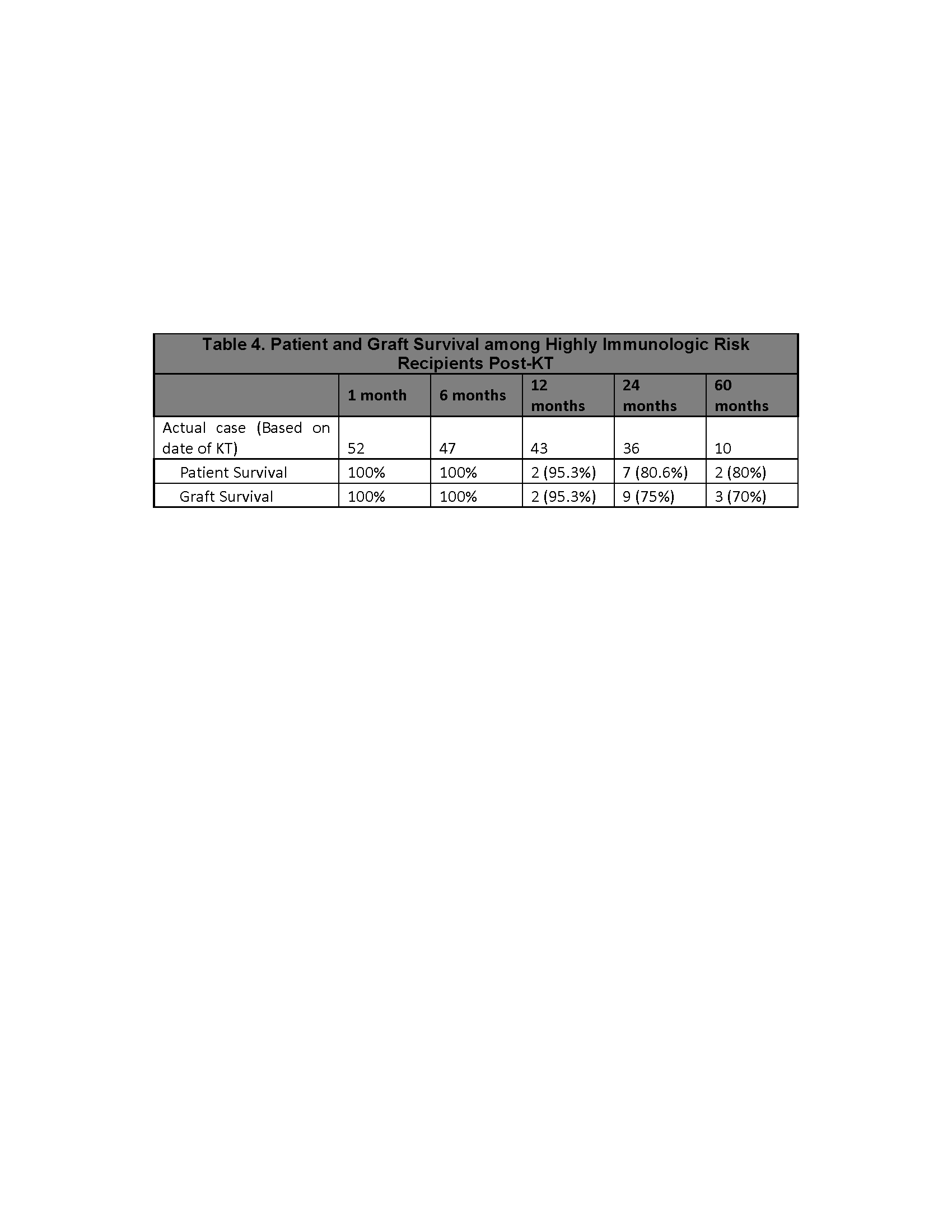
Discussion: Desensitization therapy did not confer additional risk of infection as this occurred to 26.9% of cases across all subgroups. This supports the findings of Kahwaji J et. al. that the rate of infection was similar in patients who received Rituximab+IVIG for desensitization compared with patients who did not receive Rituximab. Patients who received rATG had lower graft rejection rate compared to Basiliximab (16.7% vs 25%). This finding approximates the results of several studies like that of Brennan et. al. (15.6% vs. 25.5%, P=0.02), and Kesiraju et. al. (14.2% and 18.1%). The frequency of acute rejection is higher among DSA(+) patients and inversely, chronic rejection is more frequent among DSA(-) patients.
Conclusions: Patient and graft survival decreased over time, 95% after 1 year, 81 and 75% after 2 years, and 80 and 70% after 5 years, respectively. Infection was the most common complication regardless of desensitization history. The 5-year biopsy proven rejection was 17.3%.
