Hard-to-Place Kidney Offers: System-Level Predictors of Discard
Reinier Narvaez1,3, Jing Nie3, Katia Noyes1,3, Mary Leeman2, Liise Kayler1,2,4.
1Department of Surgery, University at Buffalo, Buffalo, NY, United States; 2Jacobs School of Medicine and Biomedical Sciences, University at Buffalo, Buffalo, NY, United States; 3Epidemiology and Environmental Health, University at Buffalo School of Public Health and Health Professions, Buffalo, NY, United States; 4Transplant and Kidney Care Regional Center of Excellence, Erie County Medical Center, Buffalo, NY, United States
Background: Deceased-donor kidney discard rates remain high. Inefficiencies in the allocation of hard-to-place kidneys may be contributing to discard suggesting that system-level factors represent opportunities to improve placement.
Methods: We analyzed DonorNet® data of consecutive deceased-donor non-mandatory share primary kidney-only offers to adult candidates at our center and beyond between July 1, 2015 and March 31, 2016 to identify system- level risk factors of discard independent of donor quality. Discard was defined as non-transplantation at our or subsequent transplant centers. Exclusions were HCV/HBV (n=14), blood type AB (n=20), and donor< 1 year (n=25) based on low candidate waitlist size.
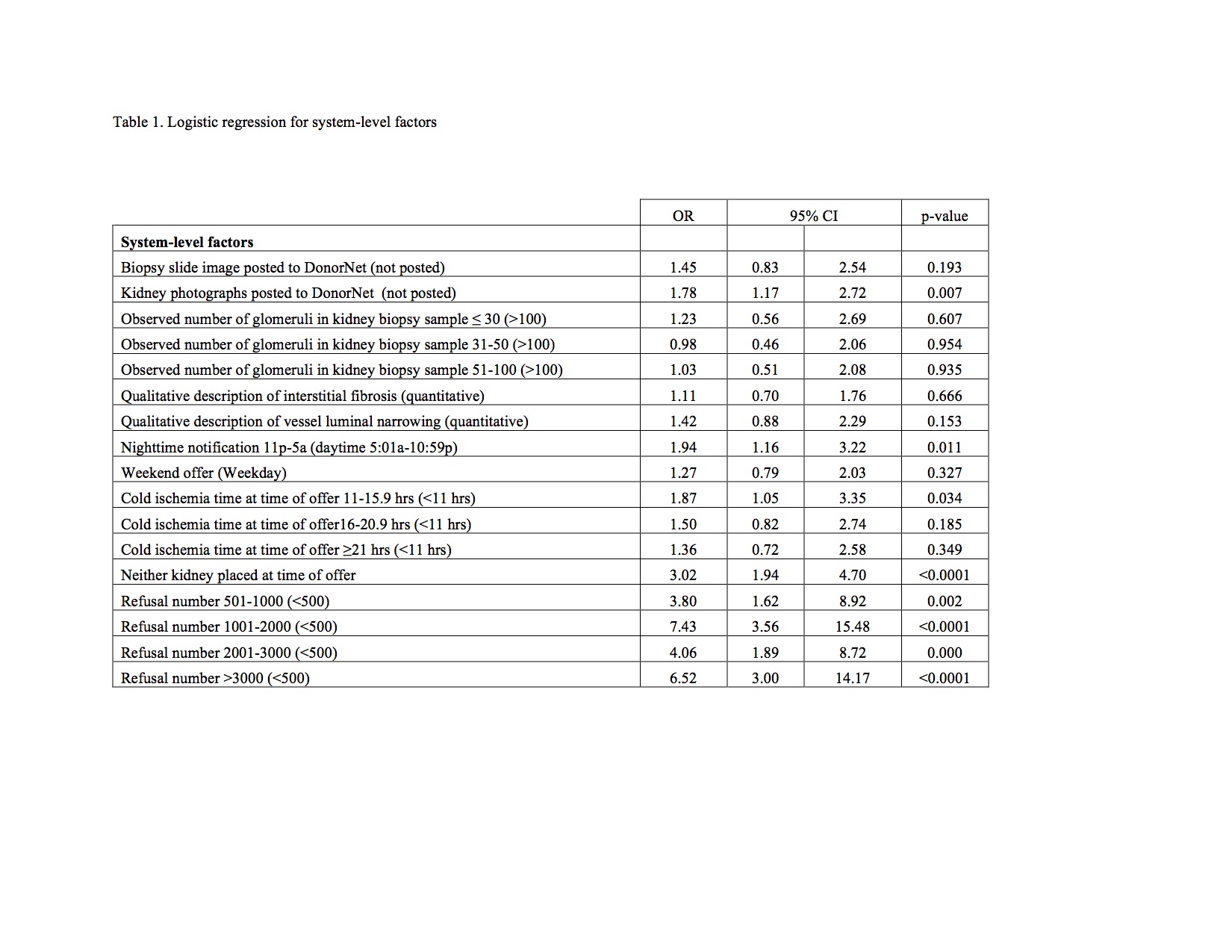
Results: Of 456 individual kidney offers, from 296 donors, 73% were discarded. Most were national (93%) offers from KDPI 35-85% (n=233) or > 85% (n=208). Each system-level factor (Table 1) was separately entered into the multivariate model containing donor-level factors and those that remained significant independent factors associated with discard were increasing offer cold ischemia time (11-15 hours: aOR 2.07, 95%CI 1.08-3.97; 16-20 hours: aOR 2.33, 95%CI 1.15-4.75; ≥21 hours, aOR 2.82, 95%CI 1.30-6.13), increasing refusal number (501-1000, aOR 2.23, 95%CI 0.77-6.44; 1001-2000, aOR 6.68, 95%CI 2.78-16.07; 2001-3000, aOR 2.39; >3000, aOR 5.34, 95%CI 2.09-13.62), night-time offer (aOR 2.19; 95%CI 1.18-4.10), and neither kidney placed at time of offer (aOR 2.74, 95%CI 1.60-4.72). Absence of kidney picture was borderline significant (aOR 1.61, 95%CI 0.97-2.67).
Conclusion: System-level factors regarding allocation efficiencies and information quality influence discard and should be considered to inform future interventions.