
Non-Immunologic Pairing of Kidney Transplant Donors and Recipients: How Important is HLA Match Status?
Amanda Miller1, Bryce Kiberd1, Karthik Tennankore1.
1Department of Medicine, Division of Nephrology, Dalhousie University, Halifax, NS, Canada
Currently, allocation preference in deceased donor kidney transplantation is given to donors and recipients (D/R) with 0 human leukocyte antigen (HLA) mismatches (MM), with non-immunologic matching between D/R rarely considered. Thus, the primary aim for this study was to determine if suboptimal pairing at five D/R loci (age, race, sex, weight and CMV serostatus) results in an increased risk of kidney graft failure, how this impact relates to HLA MM, and if HLA MM modifies this effect.
The association of D/R match with death-censored graft loss was explored using deceased donor recipients from 2000-2014 identified through the Scientific Registry of Transplants Recipients. A Cox regression coefficient-based scoring system was used to assign points to each D/R pairing. Points were totaled across all five D/R loci and overall match was categorized as favorable (< 0), moderate (0 to < 8), or poor (≥ 8), with cut points chosen to create relatively even tertiles. D/R match groups were stratified by HLA match (favorable (0MM) or poor (1-6MM)). Time to graft loss was evaluated using multivariable Cox Proportional Hazards models adjusting for known literature predictors of graft loss. The interaction between HLA MM and D/R pairing was assessed to determine if HLA MM modifies the association between D/R pairing and graft outcome.
17,786 of 107,041 kidney transplant recipients developed death-censored graft failure. D/R matching was a stronger predictor of graft failure than HLA MM. The highest HRs for graft failure were observed for poorly matched D/R, irrespective of HLA MM (HR 3.50 95% CI [3.18-3.85]; HR 2.73 95% CI [2.40-3.11] for poor and favorably matched HLA, respectively). Even with suboptimal HLA match, the risk of graft loss was mitigated for those with a favorable D/R match (HR 1.51 95% CI [1.37-1.66]). Both D/R match and HLA MM were independently associated with the outcome of interest and and the interaction between D/R match and HLA MM was significant.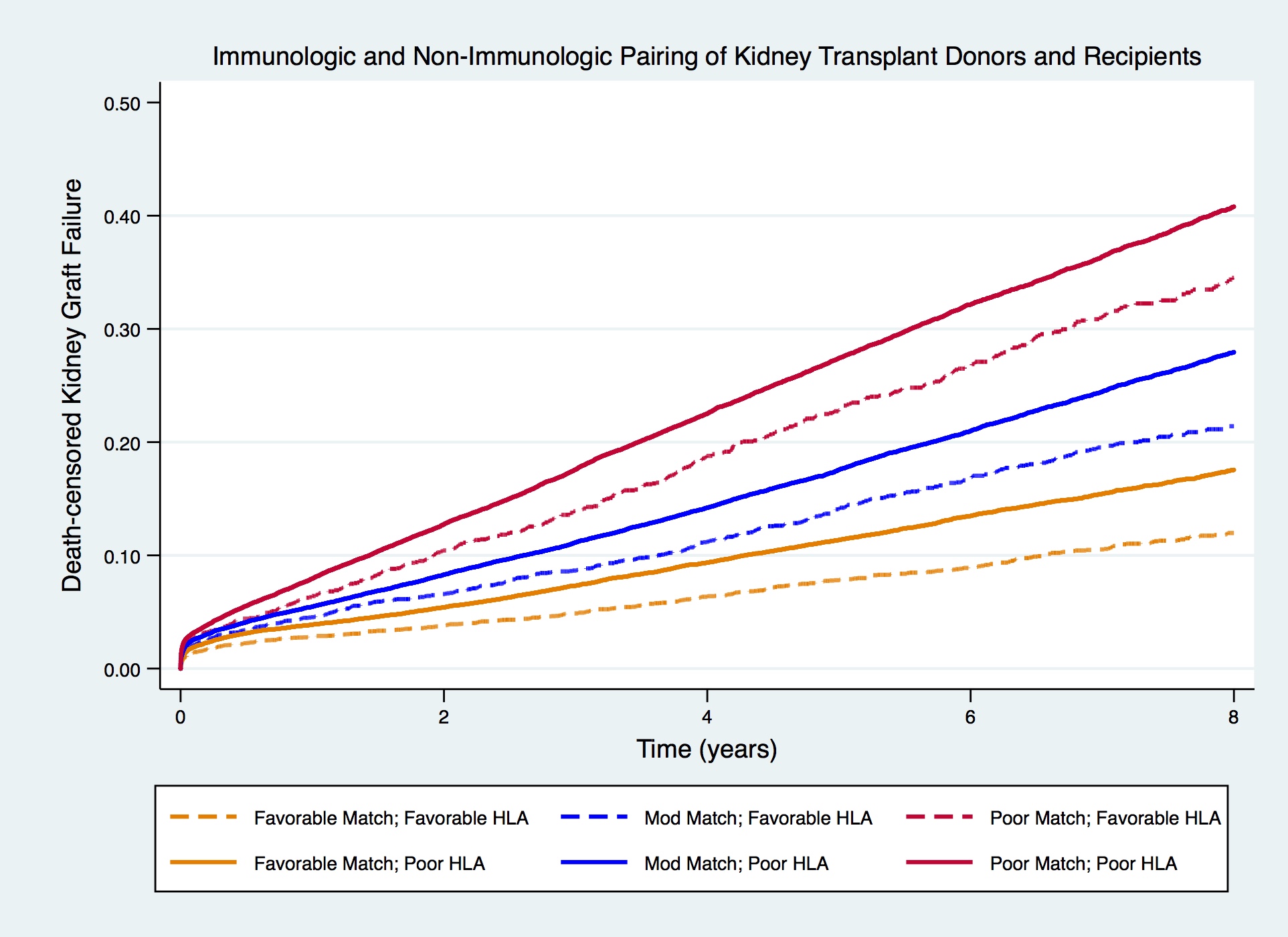
In conclusion, non-immunologic D/R matching is a stronger predictor of death-censored graft failure than is HLA match status. HLA MM modifies this association.
