Delta PD-1 Expressed M2 Macrophages Promote Liver Tumor Recurrence after Transplantation
Wai Ho Oscar Yeung1, Li Liu2, Zhi Wei Chen2, Chung Mau Lo1, Kwan Man1.
1Surgery, The University of Hong Kong , Hong Kong, Hong Kong; 2AIDS Institute and Department of Microbiology, The University of Hong Kong , Hong Kong, P.R. China
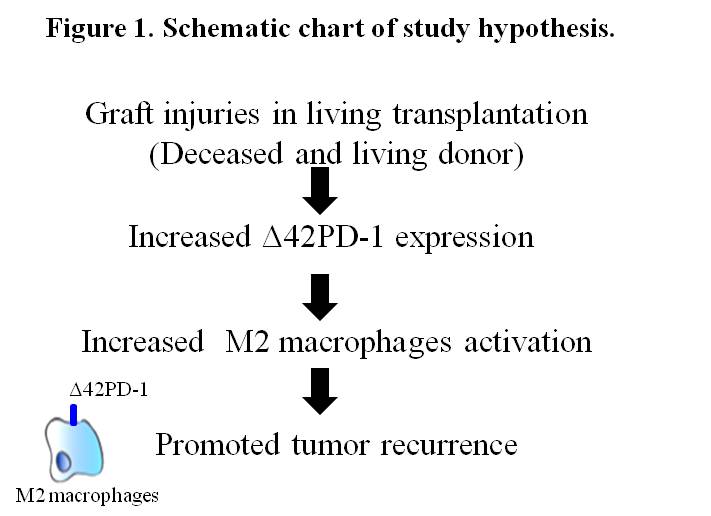
Introduction: Hepatocellular Carcinoma (HCC) is one of the dominant malignancies worldwide and become the primary cause for liver transplantation. Despite its effectiveness, tumor recurrence remains to be a challenge for liver transplantation especially in patients received living donor grafts. Macrophages are key immune cells mediating the inflammatory responses during injuries. Our group previously reported that a subpopulation of macrophages (M2) enhanced tumor metastasis and contributed to poor relapse free survival in HCC patients received curative hepatectomy. Currently, the implications as well as activation mechanisms of these cells in liver transplantation are unknown. Our preliminary evidences indicated the accumulation of a subset of M2 macrophages, expressed with Δ42PD-1, a natural isoform of a immune regulator PD-1, in the post-transplant tissues. We hypothesized that liver graft injury during transplantation activate M2 macrophages, via Δ42PD-1 mechanism, leads to tumor recurrence and poor outcome in HCC patients.
Materials and Methods: A clinical cohort of 100 HCC patients who underwent deceased (DDLT) and living (LDLT) donor liver transplantation were included. To understand its clinical implications, the expression level of tissue M2 macrophages with and without Δ42PD-1+ were examined followed by the association analyses with patients post-transplant outcomes. To investigate its roles in recurrence, Δ42PD-1+ populations isolated from patients were studied in rat tumor transplant model and in vitro co-cultivation system with HCC cells (Figure 1).
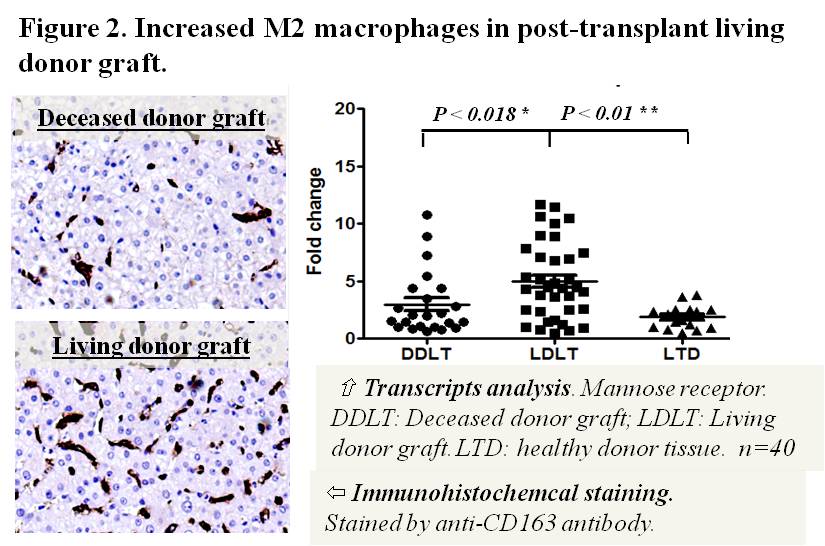
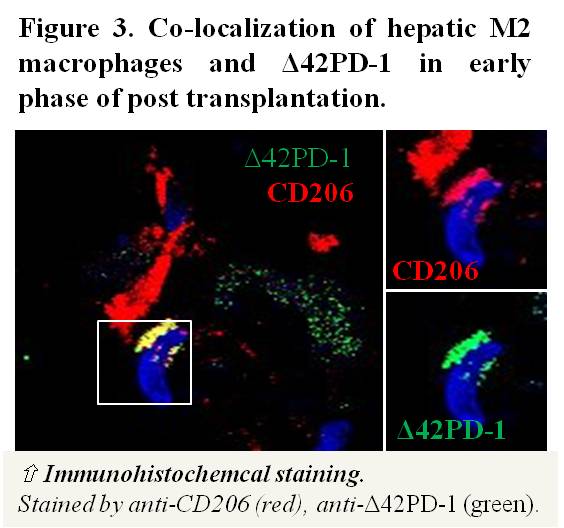
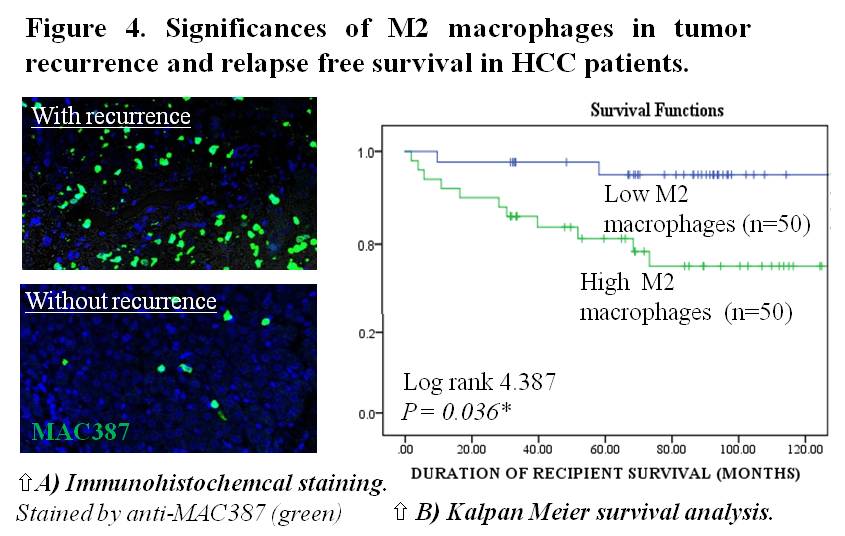
Results and Discussion: Clinically, 2.1 fold elevation of intra-hepatic M2 macrophages were found in living donor graft compared to deceased graft during the early phase of post-transplantation (P<0.01)(Figure 2). In addition, we identified the increased of Δ42PD-1 expressed in the elevated M2 sub-population (Figure 3). Further analysis indicated the M2 macrophages contributed to the higher recurrence incidences and shorter relapse free survival in patients (P=0.036)(Figure 4A and 4B). In vivo study showed that liver graft injuries significantly induced the accumulation of M2 macrophages after transplantation and resulted in larger tumor volume in the rat transplant tumor model. We showed that that Δ42PD-1[high] macrophages expressed characteristic M2 phenotypes including pro-tumor cytokine secretory profiles compared to Δ42PD-1[low] cells. Co-cultivation of Δ42PD-1[high] population with HCC cells significant increased tumor cells proliferation.
Conclusion: Here we revealed a novel cellular mechanism in promoting the post-transplant recurrence in liver transplantation. Liver graft injury induced the accumulation and activation of tumor promoting Δ42PD-1 M2 macrophages. Targeting the specific immune population and the regulatory mechanism represent a potential therapeutic strategy in attenuating tumor recurrence in HCC.