
Gut Microbiota Determines Graft Survival Outcome Through Regulation of Anti-Inflammatory and Pro-Inflammatory Responses
Yanbao Xiong1, C. Colin Brinkman1, Lauren E. Hittle2, W. Florian Fricke2, Emmanuel F. Mongodin2, Jonathan S. Bromberg1.
1CVID, University of Maryland School of Medicine, Baltimore, MD, United States; 2Institute for Genome Sciences, University of Maryland School of Medicine, Baltimore, MD, United States
Introduction: The gut microbiota plays an important role on the induction and training of the host immune system. It is unknown whether microbiota from the contrasting environments of colitic or pregnant mice are pro-inflammatory or suppressive. We hypothesized that gut microbiota from different sources could influence the survival of murine cardiac allografts through regulation of immune responses.
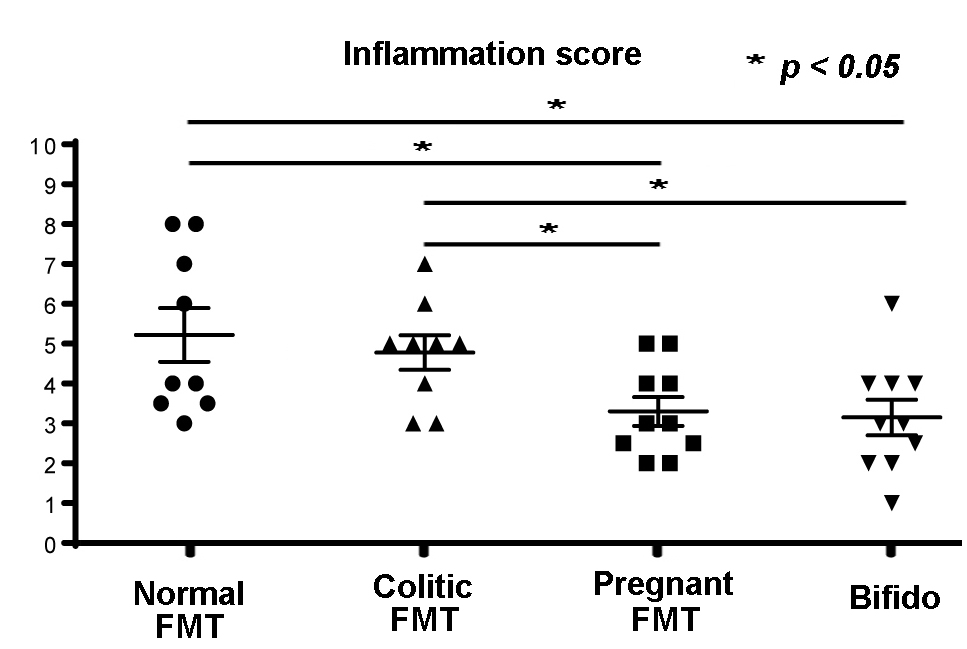
Methods: C57BL/6 mice received BALB/c vascularized cardiac allografts and fecal microbiota transfer (FMT) by oral gavage. FMT samples were from normal or pregnant C57BL/6, spontaneously colitic mice, or cultured Bifidobacterium pseudolongum (Bifido) (a dominant member of the pregnant gut microbiota). Tacrolimus was administered daily. Fecal pellets were collected weekly post-transplant and analyzed by 16S rRNA gene sequencing. Grafts were assessed for survival, harvested at days 40-60 or rejection, and assessed for inflammation by H&E and fibrosis by Masson's trichrome. Macrophage (MF) and dendritic cell (DC) lines were stimulated with purified Bifido cells and cytokine responses measured.
Results: Pregnant FMT significantly prolonged survival, and reduced inflammation and fibrosis of cardiac allografts. Normal or colitic FMT resulted in inferior survival, along with increased fibrosis and inflammation. 16S rRNA analyses demonstrated abundant Bifido in the pregnant and normal but not the colitic FMT samples. Transfer of Bifido alone also resulted in enhanced allograft survival and reduced inflammation and fibrosis. Serial 16S rRNA analyses of gut microbiota from normal, colitic, pregnant FMT, or Bifido groups, revealed significant differences in bacterial community structure (alpha- and beta-diversity). Bifido remained abundant in pregnant FMT samples for at least 40 days. In contrast, Desulfovibrio and Deferribacteraceae were more abundant in colitic samples. Microbiota community structures of the various groups became less divergent over time, but remained distinct. DC and MF lines stimulated with Bifido expressed higher levels of the anti-inflammatory cytokine IL-10 and homeostatic chemokine CCL19, but lesser amounts of the pro-inflammatory cytokines TNFa and IL-6 compared to LPS stimulated cells.
Conclusion: The gut microbiota has profound effects on host immune responses with consequences for cardiac allograft outcomes. Distinct bacterial species or genera may both alter immunity and predict graft outcomes, with Bifidobacterium species inducing anti-inflammatory effects through stimulation of DC and MF. Therapeutic targeting of the microbiota or its functions could be beneficial in reducing inflammation and subsequent graft rejection.
