The Potential of Repairing Ischemically Damaged Human Kidneys during Acellular Warm Perfusion
Lauren Brasile1, Nicholas Henry1, Bart Stubenitsky2.
1Research and Development, BREONICS Inc., Watervliet, NY, United States; 2Surgery, St. Antonius Hospital, Utrecht, Netherlands
Introduction: In previous work we demonstrated the feasibility of resuscitating oxidative metabolism of sufficient magnitude to result in restored synthetics functions in kidney allografts with as much as 2H of warm ischemic (WI) injury during an acellular warm perfusion. The restored synthetic functions lead to modulation of both injury and repair proteins in the damaged kidneys. We now report that a longer period of ex vivo warm perfusion of human DCD kidneys results in a more extensive regeneration as revealed by the observation of actual mitosis in the repairing human kidneys by 48H of warm perfusion (Figure 1). We also evaluated whether a Mesenchymal Stem/Stromal Cell (MSC) therapy could accelerate this active reparative process in the ischemically damaged human kidneys during the ex vivo warm perfusion. We hypothesized that by administering MSC directly to the renal tissue, there would be an improved opportunity for cellular repair mediated by the increased intrarenal paracrine effects.
Methods: The studies were performed using the Exsanguinous Metabolic Support (EMS) platform. Paired human kidney allografts from DCD donors (mean WI of 30 min with unknown down time in 2) were studied. Kidneys were EMS perfused with or without the addition of MSC (1x10^8). The kidneys were evaluated by histological grading, cytokine/chemokine synthesis and a panel of biomarkers indicative of DNA synthesis and cytoskeletal regeneration.
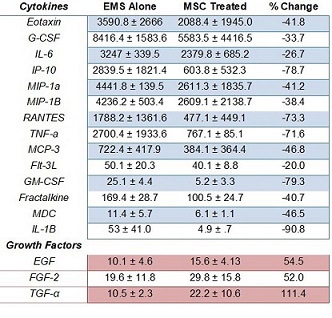
Results: The period of warm perfusion led to a significant increase in the synthesis of ATP and growth factors resulting in normalization of metabolism and the cytoskeleton during ex vivo perfusion. The addition of a MSC treatment led to a further reduction in the synthesis of inflammatory cytokines as well as an increase in the synthesis of growth factors that are associated with renal regeneration (Table 1). Toluidine Blue staining of MSC treated kidneys demonstrated a significant increase in the number of renal cells undergoing mitosis (23%) compared to EMS perfusion alone (Figure 1).
Discussion: To our knowledge, our work is the first to have achieved actual cellular regeneration while ischemically damaged human kidneys are perfused ex vivo for several days. The observation of increased growth factor synthesis is significant because the polypeptides are known to potentiate kidney function and have been shown to play an important role in vivo for the recovery of function following renal damage.
Conclusion: The observed regeneration entails: increased synthesis of ATP, reduced inflammatory response, increased synthesis of growth factors, normalization of the cytoskeleton and mitosis. The added treatment of administering MSCs further potentiated the renal repair. The ability to regenerate renal tissue ex vivo sufficiently to result in immediate function could revolutionize transplantation by helping to address the chronic organ shortage.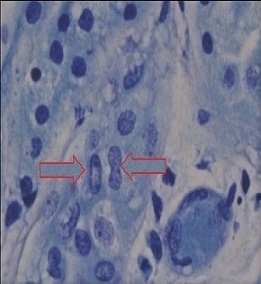
National Institute of Health - NIAID Grant # R43AI06362.
