CDC High Risk Livers Should be Used more Frequently in Pediatric Liver Transplantation
Christine Hwang1, Ali El Mokdad1, Malcolm MacConmara1.
1Surgery, University of Texas Southwestern Medical Center, Dallas, TX, United States
Introduction: Despite a discrepancy in donor liver volume in comparison to patients listed for liver transplantation, there remains hesitancy in utilizing livers from donors that are considered to be Centers for Disease Control and Prevention (CDC) high risk. We examined if this hesitancy is warranted by examining outcomes in the pediatric liver transplant population who received CDC high risk livers.
Materials and Methods: The United Network for Organ Sharing database was queried to examine outcomes in all liver transplant recipients from 1993 to 2017. The patients were then divided upon adult and pediatric (under age 18 years) status, presence of CDC high risk status or not, and era of transplantation (prior to 1999 vs. after 1999). Donor and recipient demographic data were examined, and patient and allograft survival were calculated. Kaplan Meier survival curves were generated. Categorical differences were compared using the unpaired Student's t-test and nominal variables using either the Chi Square or Fischer's exact test. A p-value of <0.05 was considered to be significant.
Results and Discussion: A total of 381 pediatric liver transplant recipients received a liver from a CDC high risk donor. The average donor age in the pediatric CDC high risk group (CDCHR) was 15.5 vs. 13.7 years (p<0.05) in the non CDC high risk group (NCDCHR). The average cold storage time in the CDCHR was 7.1 vs. 8.2 hours (p<0.05) in the NCDCHR. The average age of recipient in the CDCHR was 5.6 vs. 4.8 years (p<0.05) in the NCDCHR. The severity of illness, as defined by needed life support at the time of transplant, in the CDCHR was 11% vs. 12.7% (p=NS) in the NCDCHR, and the average MELD/PELD score in the CDCHR was 17 vs 15 (p<0.05) in the NCDCHR. The rate of recipient retransplantation in the CDCHR was lower at 7.9% vs. 14.9% (p<0.05) in the NCDCHR. When examining patient and allograft survival in all pediatric recipients who received a CDC high risk allograft, survival was significantly better in the CDC high risk group. 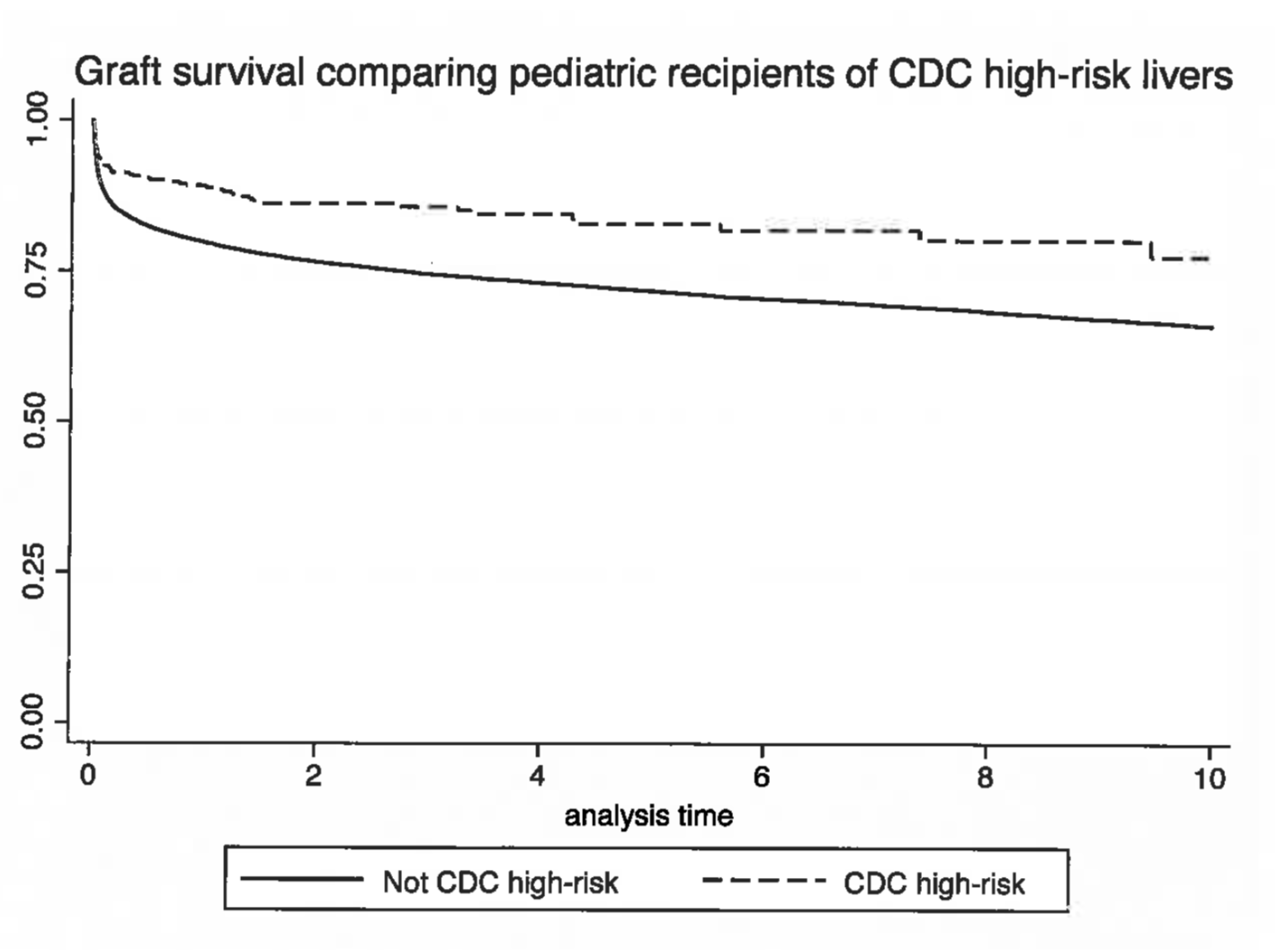
The donors in the CDCHR were significantly older with a longer cold storage time. The recipients in the CDCHR were significantly older, sicker based upon MELD/PELD, and less likely to need retransplantation. There was no transmission of any disease from donor to recipient in a recipient who received a CDC high risk allograft. Patient and allograft survival was superior when compared to those recipients who did not receive a CDC allograft, indicating that the CDC high risk liver is a safe and viable option to increase the donor pool for livers in pediatric recipients.
Conclusion: Patient and allograft survival in CDC high risk donor livers is superior to those allografts that are not considered to be CDC high risk. Use of CDC high risk liver allografts should be strongly considered to increase the organ pool for pediatric patients.
