Banff Survey on Antibody Mediated Injury in Kidney Allografts: Diagnostic Misclassification Affects the Treatment Approach
Carrie Schinstock1, Maarten Naessens2, Lynn Cornell6, Edward Kraus3, Ajda Rowshani5, Ruth Sapir-Pichhadze4.
1Von Liebig Center for Transplantation and Regenerative Medicine, Mayo Clinic, Rochester, MN, United States; 2Katholicke Universiteit Leuven, Leuven, Belgium; 3Nephrology, Johns Hopkins University School of Medicine, Baltimore, MD, United States; 4Nephrology, McGill University, Montreal , QC, Canada; 5Erasmus University, Rotterdam, Netherlands; 6Laboratory Medicine and Pathology, Mayo Clinic, Rochester, MN, United States
Background: Diagnostic misclassification has major clinical practice implications. The aims of this study were to determine how the Banff 2013 antibody-mediated rejection (ABMR) classification system is interpreted in practice and how it affects therapeutic decision making.
Methods: The Banff ABMR working group electronically surveyed clinicians and pathologists worldwide, with respondents from 6 continents. The survey consisted of six case vignettes with common ABMR scenarios. Participants were asked to provide their diagnosis and corresponding treatment approach. The respondents’ assigned diagnosis was compared to the intended Banff diagnosis (reference standard). Fisher’s exact test was used to compare categorical data.
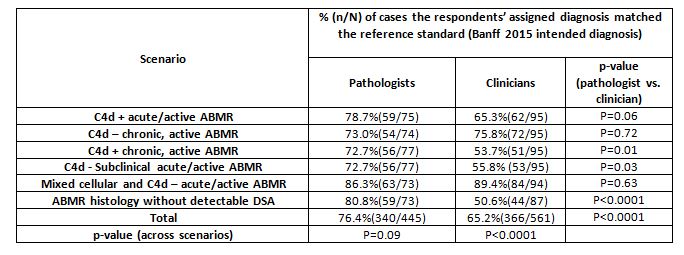
Results: A total of 95 clinicians and 83 renal pathologists participated in the survey. In 25.9% (247/953) of cases, the respondents’ assigned diagnosis differed from the reference standard. The assigned diagnosis and reference standard matched in 76.4% (340/445) of cases among pathologists and 65.2% (366/561) of the cases among clinicians. The discrepancy between the assigned diagnosis and reference standard was similar regardless of the scenario for pathologists, but differed for clinicians (Table 1). Among clinicians, this discrepancy was greatest when ABMR histology was present but DSA was undetected [only 50.6% (44/87) of diagnoses matched the reference standard]. Importantly, the clinicians’ treatment approach appeared to be linked to the assigned diagnosis. When the acute active ABMR diagnosis was assigned; specific treatment for ABMR was recommended 88.3% (234/265) of cases, but in only 71.7% (132/184) of cases when chronic ABMR was assigned, (p<0.0001). Considering the misclassification rate, acute and chronic ABMR diagnosis resulted in potentially unintended treatment in 57/325 (17.5%) and 99/332 (29.8%) of cases, respectively (p=0.002).
Conclusion: The current Banff ABMR classification scheme is vulnerable to misinterpretation in clinical practice. This potentially has major clinical consequences because the ABMR diagnosis influences therapeutic approaches. Our findings suggest a reevaluation of the Banff ABMR classification to facilitate its reproducibility and standardization when applied clinically.
Table 1. Interpretation of Banff ABMR classification in Clinical Practice