Pre-Donation Renal Function, Early Post-Donation Renal Function, and Subsequent ESRD Risk in Living Kidney Donors
Allan Massie1, Lara M Fahmy1, Macey L Henderson1, Alvin Thomas1, Jon Snyder1, Fawaz Al Ammary1, Dorry L Segev1.
1Surgery, Johns Hopkins School of Medicine, Baltimore, MD, United States
Several predonation risk factors for ESRD in living kidney donors (LKDs) have been identified. However, the relationship between predonation eGFR and long-term risk of postdonation ESRD has not been characterized. Moreover, all LKDs may not tolerate the insult of living donor nephrectomy equally well. The clinical utility of measuring early post-donation renal function is unknown.
Methods: Using national registry data from the United States (SRTR), we studied ESRD risk in 66,052 LKDs 1999-2015 who were ESRD-free 9 months post-donation and had at least one postdonation serum creatinine (SCr) reported to the registry between 3 and 9 months post-donation (6m-post eGFR), using Cox regression and adjusting for donor age, sex, race (black vs all other), 1st-degree biological relationship to recipient, and BMI. Predonation eGFR and 6m-post eGFR were calculated from donor age/race/sex/SCr using the CKD-EPI equation.To determine whether absolute post-donation eGFR or the drop from predonation to postdonation eGFR was the best predictor of post-donation ESRD, we compared models using the Akaike Information Criterion (AIC) to assess goodness-of-fit.
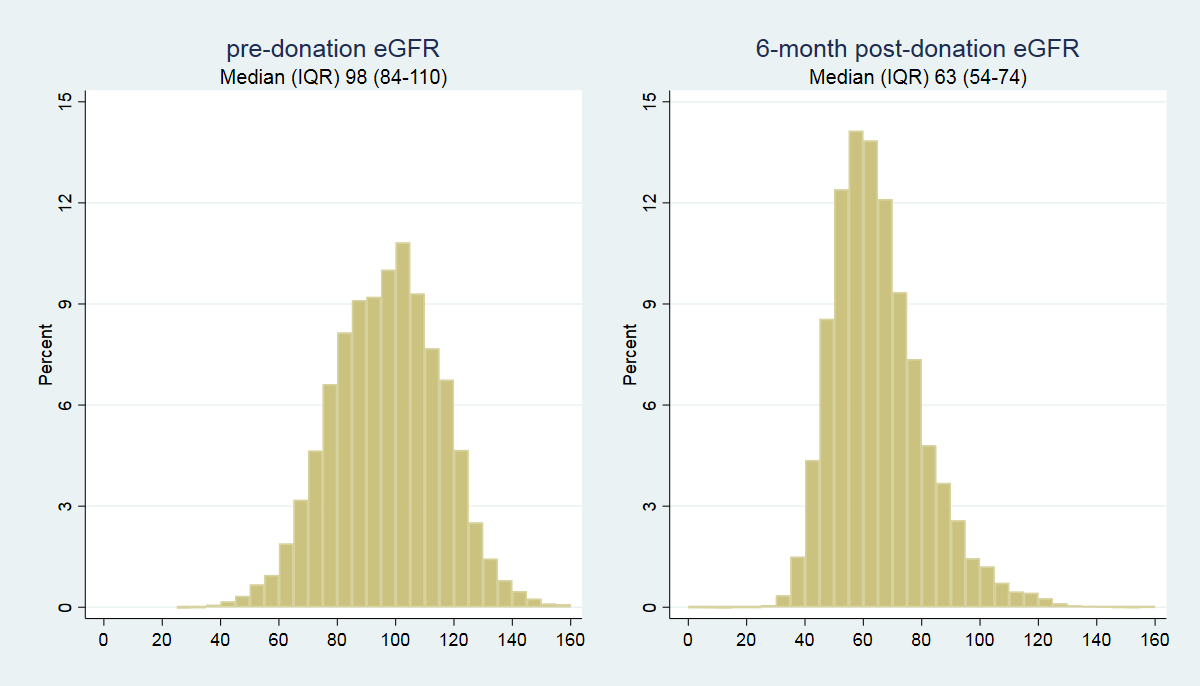
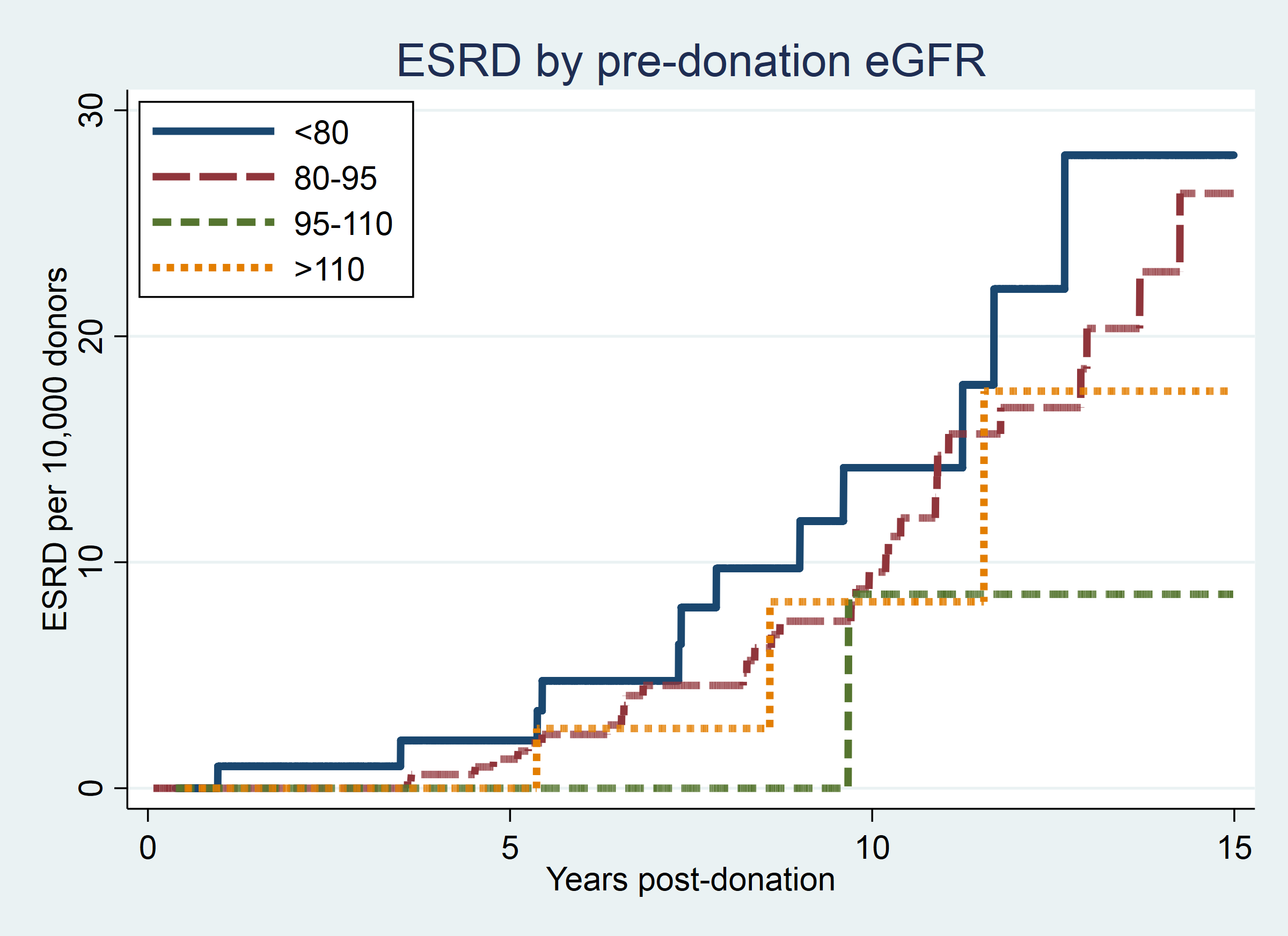
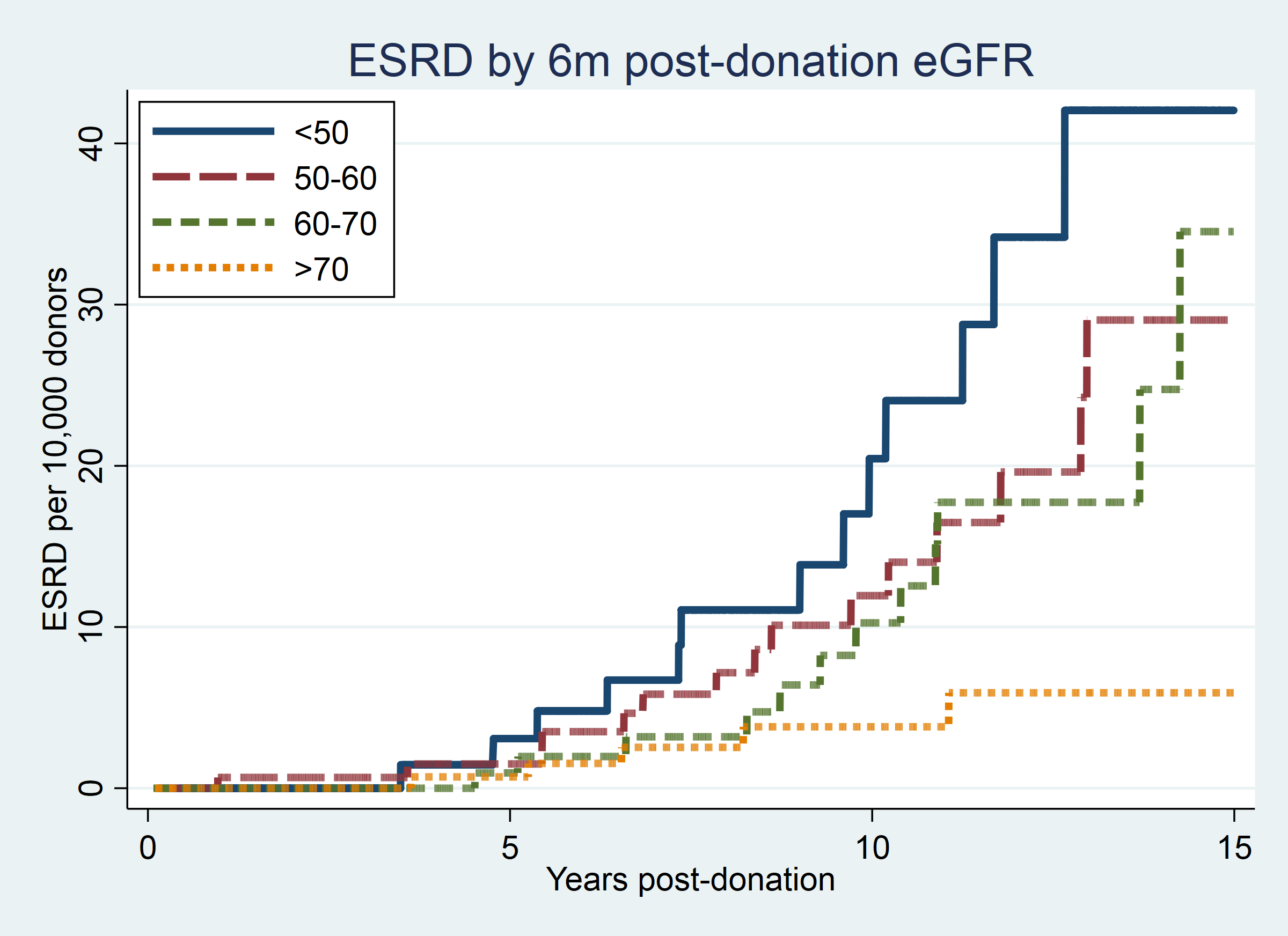
Results: Donor eGFR declined from median (IQR) 98 (84-110) mL/min/1.73 m2 predonation to 63 (54-74) mL/min/1.73 m2 6m-post (Figure 1). A 10-unit increase in predonation eGFR was associated with 17% decreased risk of ESRD (aHR=0.70 0.83 0.99, p=0.04) (Figure 2). In a separate model, a 10-unit increase in 6m-post eGFR was associated with 40% decreased risk of ESRD (aHR=0.46 0.60 0.79, p<0.001) (Figure 3). In a model including both predonation and 6m-post eGFR, the association between predonation eGFR and ESRD risk disappeared (aHR per 10u=0.79 0.98 1.21, p=0.9) while the association between 6m-post eGFR and ESRD risk remained the same (aHR per 10u=0.44 0.61 0.83, p<0.001), suggesting that the association between predonation eGFR and ESRD is fully mediated by 6m-post eGFR.
After adjustment, the AIC of a model of 6m-post eGFR and ESRD (AIC=807.69) was substantially lower than the AIC for a model of pre-to-post eGFR decline and ESRD (AIC=822.02), suggesting that absolute postdonation eGFR is a better predictor of postdonation ESRD risk than the decline from predonation to 6m-post.
Conclusions: Both predonation and 6m-post eGFR are inversely associated with postdonation ESRD risk in LKDs. The association between predonation eGFR and ESRD represents screened candidates who have been cleared to donate; as such, donors with low predonation eGFR who have passed screening may be better candidates than members of the general population with the same predonation eGFR. Careful monitoring of early postdonation eGFR is essential to provide adequate postdonation care and counseling.
NIDDK R01DK096008 (PI: Segev). NIDDK K01DK101677 (PI: Massie).
