Obesity Is Associated with Increased Risk of Mortality among Living Kidney Donors
Rhiannon Reed1, Allan B Massie2, Deirdre Sawinski3, Paul A MacLennan1, Brittany A Shelton1, Margaux N Mustian1, Deanna M McWilliams1, Vineeta Kumar4, Roslyn B Mannon4, Robert Gaston4, Dorry L Segev2, Cora E Lewis4, Jayme E Locke1.
1Surgery, University of Alabama at Birmingham, Birmingham, AL, United States; 2Surgery, Johns Hopkins University, Baltimore, MD, United States; 3Medicine, University of Pennsylvania, Philadelphia, PA, United States; 4Medicine, University of Alabama at Birmingham, Birmingham, AL, United States
Background: Living kidney donor (LKD) demographics have changed, and United States transplant centers have relaxed selection criteria to include LKDs who are obese. Recently, it has been demonstrated that obese LKDs have increased risk for post-donation end-stage renal disease (ESRD) compared to their non-obese counterparts. However, no study to-date has examined post-donation mortality risk among obese LKDs.
Materials and Methods: 119,769 LKDs (1987-2013) were studied from the Scientific Registry of Transplant Recipients, a comprehensive registry of organ donors and recipients in the US since 1987. Obese LKDs were defined as donors with body mass index (BMI) ≥ 30kg/m2 at the time of donation. Multiple imputation using chained equations were used to impute BMI, systolic and diastolic blood pressure, relationship to recipient, estimated glomerular filtration rate, and history of cigarette smoking when missing. Maximum follow-up time was 28 years. Main outcome measures included cumulative incidence (presented as crude estimates and smoothed Kaplan-Meier curves averaged from multiply imputed datasets) and risk of mortality in Cox proportional hazards regression, with development of ESRD treated as a time-varying covariate. Risk for ESRD was modeled separately for obese and non-obese donors.
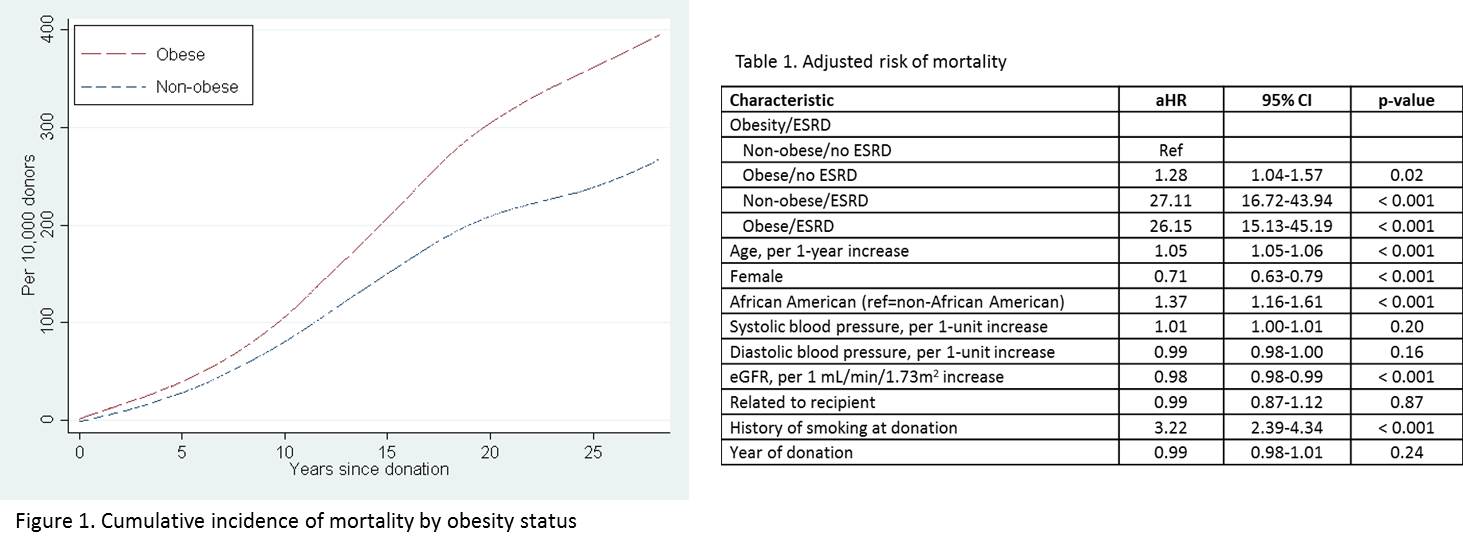
Results: Compared to non-obese LKDs, obese LKDs were more likely male (43.1% vs. 39.2%), African American (16.4% vs. 11.1%), and to have higher mean systolic blood pressure (124.1 vs. 119.9 mmHg). Unadjusted risk of mortality at 25 years post-donation was 304.3 per 10,000 for obese LKDs and 208.9 per 10,000 in their non-obese LKD counterparts (Figure). In the absence of ESRD development, the risk of mortality among obese LKDs was 1.3-fold higher than non-obese LKDs (adjusted hazard ratio (aHR): 1.28, 95%CI: 1.04-1.57, p=0.02). For donors who developed ESRD, the risk of mortality was similar, regardless of obesity status (non-obese/ESRD aHR: 27.11, 95% CI: 16.72-43.94, p < 0.001; obese/ESRD aHR: 26.15, 95% CI: 15.13-45.19, p < 0.001). (Table)
Conclusions: Compared with non-obese LKDs, LKDs who are obese at the time of donation had an increased risk of mortality within 28 years of donation. However, the presence of obesity at donation does not appear to confer additional mortality risk for donors who develop post-donation ESRD. These findings may help to inform selection criteria and discussions with persons considering live kidney donation.
National Institutes of Health 5K23DK103918.
