Clinical Utility and Interpretation of CKD Stages in Living Kidney Donors
Allan Massie1, Macey L Henderson1, Jon Snyder1, Fawaz Al Ammary1, Dorry L Segev1.
1Surgery, Johns Hopkins School of Medicine, Baltimore, MD, United States
Current definitions of chronic kidney disease (CKD) staging define any individual with eGFR below 60 mL/min/1.73 m2 as having stage 3 or higher CKD. Nearly half of living kidney donors (LKDs) have post-donation eGFR below this threshold, but the clinical interpretation of eGFR<60 in this population is unknown, and some advocates for LKDs have objected to applying the "CKD" label to such a large proportion of LKDs. Evidence of risk associated with decreased post-donation eGFR is needed to inform international guidelines and best practices for donor followup and care management.
Methods: Using national registry data from the United States (SRTR), we studied end-stage renal disease (ESRD) risk in 67,571 LKDs 1999-2015 with at least one postdonation serum creatinine (SCr) reported to the registry. We calculated eGFR using the CKD-EPI equation. Measurements with eGFR<15 were excluded from analysis. Donors were followed through 16 years post-donation or administrative censorship on 12/31/2015. We modeled the association between eGFR category (≥60, 45-59, 30-44, 15-30, corresponding to no CKD, CKD stage 3, stage 4A, and stage 4B) using Cox regression with eGFR category as a time-varying exposure and adjusting for donor age, sex, race (black vs nonblack), BMI, and 1st-degree biological relationship to recipient.
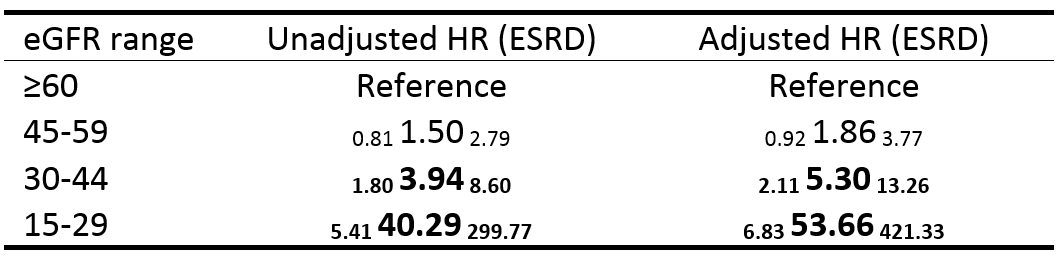
Results: A total of 117,051 CKD measurements were reported at median (IQR) 11 (4-14) months post-donation (90th percentile 25 months post-donation). Of these, 33.9% were in the range 45-59, 5.7% were in the range 30-45, and 0.8% were in the range 15-29. In an unadjusted model, eGFR 30-45 was associated with 3.9-fold higher risk of ESRD compared to donors with eGFR≥60 (HR=1.80 3.94 8.60, p<0.01) and eGFR 15-29 was associated with 40-fold higher risk (HR=5.41 40.29 299.77, p<0.001) (Table). After adjustment, these associations persisted with 5.3-fold higher risk for eGFR 30-45 (aHR=2.11 5.30 13.26, p< .001) and 54-fold higher risk for eGFR 15-29 (aHR=6.83 53.66 421.32, p<0.001). Donors with eGFR 45-60 had elevated risk but the association was not statistically significant (unadjusted HR=0.81 1.50 2.79, p=0.2; aHR=0.92 1.86 3.77, p=0.08).
Conclusions: Associations between eGFR category and subsequent ESRD risk are less strong in LKDs than in the general population, and the categorization of eGFR 45-60 as "CKD stage 3" may not be clinically meaningful among LKDs. Nevertheless, eGFR category is associated with subsequent ESRD risk among donors with eGFR<30, and our results support current guidelines recommending longitudinal followup of renal function in living kidney donors.
NIDDK R01DK096008 (Segev). NIDDK K01DK101677 (Massie).
