Aravind Cherukuri, United States has been granted the TTS Young Investigator Scientific Award
Prospective Multicenter Validation of Human Transitional B cell Cytokines as a Predictive Biomarker in Renal Transplantation
Aravind Cherukuri1, Dominik Chittka1, Akhil Sharma1, Rajil Mehta1, Sundaram Hariharan1, Hans Stauss3, Mark Harber2, Fadi Lakkis1, Ciara Magee2, Alan Salama2, David M Rothstein1.
1Thomas E. Starzl Transplant Institute, University of Pittsburgh, Pittsburgh, PA, United States; 2Royal Free Center For Nephrology, UCL, London, United Kingdom; 3UCL Institute of Immunity and Transplantation, UCL, London, United Kingdom
Introduction: In renal transplantation, non-invasive biomarkers are needed to identify patients at risk for poor outcomes and guide pre-emptive therapy. In this prospective multicenter study, we assessed B cells and their cytokines as a predictive biomarker.
Methods: Based on prior data, we tested the ratio of IL-10:TNFα expression in peripheral blood T1 transitional B cells (T1B) 2-4mo post-transplant, to perform as an early biomarker of clinical course. (Cytokines were examined by flow cytometry after 24hr stimulation with CD40L & CpG).
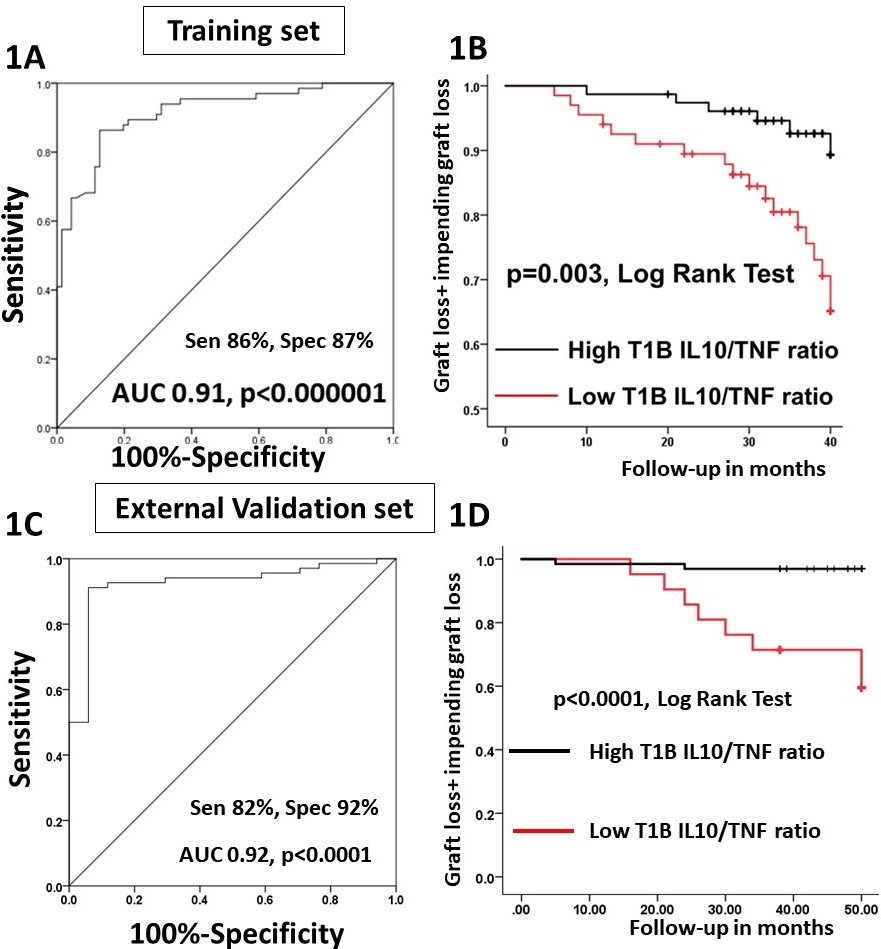
Results: 165 patients (transplanted in 2013-14) with serial biopsies (Bxs) (including 3&12mo protocol Bxs + for-cause Bxs) and serial blood draws (0, 1, 3, 6 & 12mos) served as the training set. Immunosuppression utilized Thymoglobulin induction followed by MPA+TAC maintenance. A low T1B IL10:TNFα ratio at 3mo predicted acute rejection (AR) within the 1st yr (Fig1A). Notably, in patients with a normal Bx at 2-4mo, a low T1B cytokine ratio strongly predicted late AR (6-12mo; AUC 0.9, p<0.0001) with a lead time of > 7mo in 80% of the patients. These data were validated in an independent internal cohort (2015, n=74). Further, a low T1B cytokine ratio was associated with IFTA (12 mo) and graft loss/impending graft loss (eGFR<30ml/min & >30% fall from baseline) at 4yrs (Fig1B). The predictive value of this biomarker was not influenced by either opportunistic viral infections or by non-adherence.
Next, T1B cytokine ratio was validated in an external cohort (n=100) from the UK. Immunosuppression utilized Basiliximab induction followed by TAC+MMF maintenance. As protocol Bxs were not performed in this cohort, all AR was clinical. Again, the T1B cytokine ratio at 3mo strongly predicted AR within the 1st yr (Fig1C), and was associated with significantly greater graft loss/impending graft loss (Fig1D).
B cells in high-risk patients express excessive TNFα relative to IL-10. Culture of B cells from such patients with α-TNF, reduced their TNFα and increased their IL10 expression. Such B cells subsequently suppressed autologous ∝-CD3 stimulated T cell TNFα while increasing IL10 expression. Thus, TNF blockade restored a normal B cell cytokine balance (Breg activity) in high-risk patients. Finally, α-TNF inhibited in vitro differentiation of B cells to plasma cells, reduced their Ab secretion, and selectively increased their IL-10 expression.
Conclusion: Thus, T1B IL10:TNFα ratio (2-4 mo) was tested and validated as a strong biomarker for subsequent renal allograft rejection and clinical course. Importantly, our data not only identifies patients in need of pre-emptive therapy, but provides rationale for therapeutic intervention based on TNF blockade.
American Society of Transplantation. Roche Organ Transplant Reseacrh Foundation.
