Early Outcomes and Risk Factors for Kidney Transplantation with Controlled Circulatory Death Donor (cDCD) in a Nationwide Strategy. Spanish Multicentre SENTRA-GEODAS-Group
Jose Portoles1, Maria Jose Perez-Saez2, Dario Janeiro1, Domingo Hernandez3, Javier Juega4, Francisco Moreso5, Naroa Maruri6, Paula Lopez1, Eduardo Melilli7, Maria Luisa Rodriguez-Ferrero8, Dolores Navarro9, Erika de Souza10, Rosalia Valero11, Maria Auxiliadora Mazuecos12, Alez Gutierrez13, Isabel Perez-Flores14, Julio Pascual2.
1Nephrology, H.U.Puerta de Hierro, Majadahonda, Spain; 2Nephrology, H.U. del Mar, Barcelona, Spain; 3Nephrology, H.U. Carlos Haya, Malaga, Spain; 4Nephrology, H.U. Germans Trial y Pujol, Barcelona, Spain; 5Nephrology, H.U. Vall de Hebron, Barcelona, Spain; 6Nephrology, HU de Cruces, Bilbao, Spain; 7Nephrology, H.U de Bellvitge, Barcelona, Spain; 8Nephrology, HU Gregorio Marañon, Madrid, Spain; 9Nephrology, HU Reina Sofia, Cordoba, Spain; 10Nephrology, HU Clinic, Barcelona, Spain; 11Nephrology, HU Marques de Valdecilla, Santander, Spain; 12Nephrology, H.U.Puerta del Mar, Cadiz, Spain; 13Nephrology, H.U.Miguel Servet, Zaragoza, Spain; 14Nephrology, H.U.Clinico San Carlos, Madrid, Spain
Spanish Multicentre SENTRA-GEODAS-Group.
Background: Controlled donation after circulatory death (cDCD) programs are running in US and some European countries has recently started on it. National transplant organization (ONT) has developed a nationwide program in Spain from Jan-2012 and 45 Centers had progressively joined by Dec2016 (1.0437 cDCD Kidney transplants-KTx). 21 centers have entered our study group. We present here main results and clinical outcomes.
Study: prospective multicentre . Systematic inclusion of every KTx from cDCD at joined units. Local center surgical procedures and inmunosuppressive protocols.
Results: We included 335 cDCD, donors aged 57,5 [19-81] year who have died mainly due to CV events (72%). 77 transferred and implanted in centers out of our group. Use of extended criteria donnors has increased progresively. During the last 5 years (2012-2016), 566 ESRD pacients receive a KTx (56.5y [19-83]), for 91.9% of them were the first KTx. Immunosuppression regimen included 98,8% induction (Thymoglobulin 67,1%/Basiliximab 32,3) plus prednisone-MMF-Tacrolimus (83,1%) or mTOR (6,9%). Median Cold ischemia time (CIT) was 12,3h and warm IT 24min. Median HLA-mismatch was 4 [0-5].
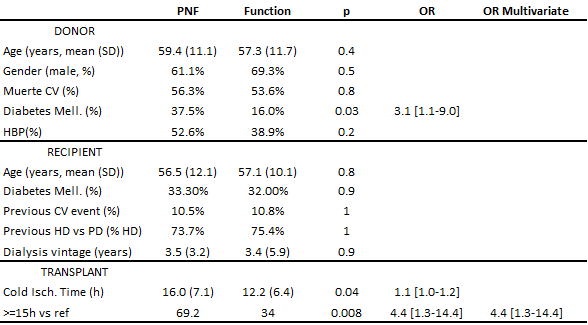
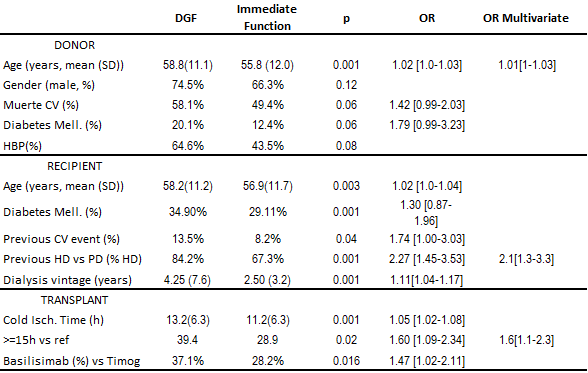
Clinical outcomes: Primary graft failure (PGF) rate was 3,4% mainly associated to preservation or vascular problems, no single hyperacute rejection case. Delayed graft function (DGF) was defined as dialysis use on 1st week after KTx. In spite of DGF rate of 48.8% and after a mean follow-up of two years (1-5 year). The death censored graft survival was 97,4% at 1 yr and 95.7% at 2 yr, graft and patient survival was 94.1% at 1 yr and 91.8 at 2 yr (Kaplan-Meier). Risk Factor associated to outcomes are summarized on Tables 1-2.
Conclusions: KTx with cDCD present higher DGF than historic reference for brain death donor but similar PGF rate and patient or graft survival rates. CIT is the only modifiable risk factor for DGF and PGF. Our results aim us to promote this cDCD all over the country.
Co-Founded by REDInREN ISCIII; FRIAT Kidney Foundation and unrestricted grant from Astellas, Novartis and Sanofy trought Research Institute of Puerta de Hierro Hospital-Segovia Arana.
