Association between Liver Perfusate Natural Killer Cellular Subset from Deceased Brain Donors and Acute Cellular Rejection after Liver Transplantation Procedure: Single Center Analysis.
Duilo Pagano1, Ester Badami2, Rosa Liotta3, PierGiulio Conaldi2, Alessandro Tropea1, Fabio Tuzzolino4, Angelo Luca3, Salvatore Gruttadauria1.
1Department for the Study of Abdominal Diseases and Abdominal Transplantation, Institute for Transplantation and Advanced Specialized Therapies (IRCCS-ISMETT), Palermo, Italy; 2Department of Laboratory Medicine and Advanced Biotechnologies, Institute for Transplantation and Advanced Specialized Therapies (IRCCS-ISMETT), Palermo, Italy; 3Department of Diagnostic and Therapeutic Services, Institute for Transplantation and Advanced Specialized Therapies (IRCCS-ISMETT), Palermo, Italy; 4Research Office, Institute for Transplantation and Advanced Specialized Therapies (IRCCS-ISMETT), Palermo, Italy
Background: Our study focuses on the cytofluorimetric examination of a monocentric series of consecutive liver perfusates (LPs) after whole graft washout in consecutive series of adult deceased brain donors (DBDs) and the predicting role of Natural Killer (NK) cell subset on the biopsy-proven acute cellular rejections (ACRs) after liver transplants (LTs).
Methods: NK, T cells and Mucosal-associated invariant T (MAIT) cells were purified by flow cytometry using CD3, CD4, CD8 and CD56 from LPs and concentrations and phenotypes were matched with DBD characteristics to determine the relative percentages of T and NK cells. The retrospective study was performed by analyzing indications, timing, surgical techniques and outcomes of consecutive patients underwent LT between 2010 and 2014 in our centre.
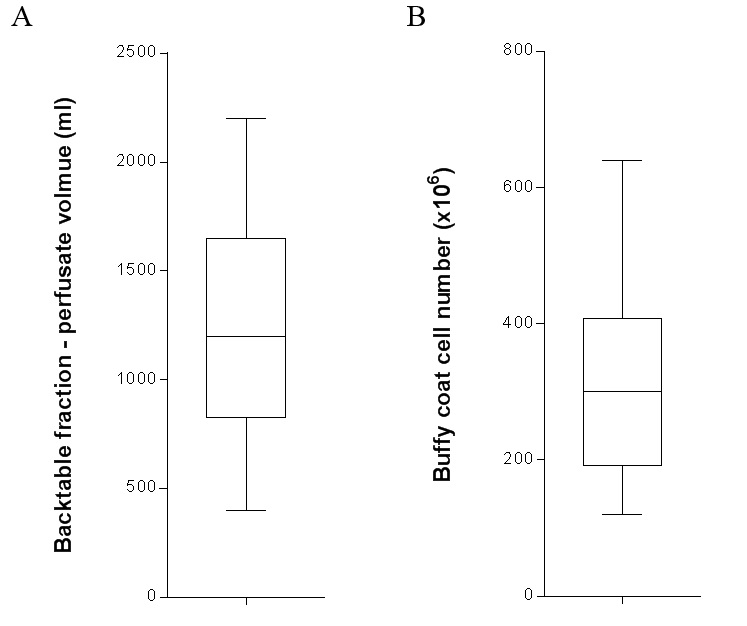
Results: LPs were collected during the back-table surgical time after the procurement procedures for 47 DBD for adult recipient. (Figure 1)
NK cell subset was strictly related to younger donor age (p = 0.003) and higher body mass index (BMI) (p = 0.01). At multivariate analysis, donor BMI was associated with reduced percentage of NK obtained by LP of DBDs (OR, -0.3% CI, 0.58-0.95, p = 0.01). A picture of severe-moderate biopsy-proven ACR was detected in 7 recipients underwent LT using whole liver allografts procured by DBDs. A significative association was observed between the quote of NK cell under the median value of NK cell LP subset (33.4%) and the evidence of severe-moderate ACR (p = 0.04).
Conclusion: Based on our experience a novel potential role of T and NK cells could be determined in ACR after LT from DBD, and this might be of high relevance for liver graft procurement and immunosuppression management.
