Post-Liver Transplant (LT) Early Allograft Dysfunction (EAD) is Associated with Lack of Post-LT Renal Recovery
Hani Wadei1, Kristopher Croome1, David Lee1, Lorraine Mai1, Burcin Taner1, Andrew Keaveny1, Martin L Mai1.
1Transplant, Mayo Clinic, Jacksonville, FL, United States
Mayo Clinic Collaborative in Transplant Research and Outcomes.
The effect of EAD on post-LT renal recovery in recipients on renal replacement therapy (RRT) at time of LT is unknown. Data on 69 primary LT recipients (41 with and 28 without history of renal dysfunction) who were on RRT for a median (range) of 9 (1-41) days prior to LT were retrospectively analyzed. EAD was defined by the presence of one or more of the following: 1) total bilirubin ≥10 mg/dl on LT day 7, 2) international normalized ratio (INR) ≥1.6 on LT day 7 and 3) alanine aminotransferase (ALT) or aspartate aminotransferase (AST) ≥2000IU/mL within the first 7 post-LT days. Renal dysfunction was defined as creatinine ≥1.5mg/dl in the 3 months prior to RRT initiation. Primary outcome was renal non-recovery defined as RRT requirement 30 days after LT.
Results: 22 (32%) patients did not recover renal function and 21 (30%) patients developed post-LT EAD. Factors associated with lack of renal recovery are demonstrated in Table 1.
|
Renal recovery (n=47) |
No Renal recovery (n=22) |
P | |
|---|---|---|---|
| Age at LT (years) | 54 ± 11 | 57 ± 8 | 0.3 |
| % Male gender | 57 | 68 | 0.4 |
| % HCV | 28 | 36 | 0.6 |
| % Diabetes mellitus | 30 | 45 | 0.2 |
| % Hypertension | 32 | 50 | 0.1 |
| MELD at LT | 35 ± 8 | 36 ± 7 | 0.6 |
| Pre-LT creatinine (mg/dl) | 1.4 ± 0.5 | 2.1 ± 1.4 | 0.04 |
| % pre-RRT renal dysfunction | 55 | 68 | 0.3 |
| RRT days | 8 (1-41) | 13 (1-36) | 0.3 |
| Donor risk index | 1.6 ± 0.5 | 1.5 ± 0.3 | 0.2 |
| % DCD | 15 | 14 | 0.9 |
| Cold ischemia time (hours) | 6.9 ± 1.7 | 6.6 ± 1.7 | 0.5 |
| Warm Ischemia time (mins) | 32 ± 9 | 34 ± 15 | 0.5 |
| Operative time (mins) | 260 ± 90 | 266 ± 117 | 0.8 |
| % EAD | 21 | 50 | 0.016 |
| % Re-exploration within 1-month post-LT | 15 | 27 | 0.2 |
| 1-month average tacrolimus level (ng/ml) | 5.1 ± 3.0 | 4.8 ± 3.0 | 0.7 |
EAD was more common in the renal non-recovery group (50% versus 21%, P=0.016). Multivariate logistic regression analysis demonstrated that EAD (OR: 7.25; CI: 2.0-25.8, P=0.002) and baseline serum creatinine (OR: 3.37; CI: 1.4-8.1, P=0.007) were independently associated with renal non-recovery. History of renal dysfunction, duration of renal dysfunction and duration of RRT were not related to renal recovery (P>0.2 for all). The 30-day post-LT probability of renal recovery was 48% in the EAD group and 77% in the no EAD group (P=0.02).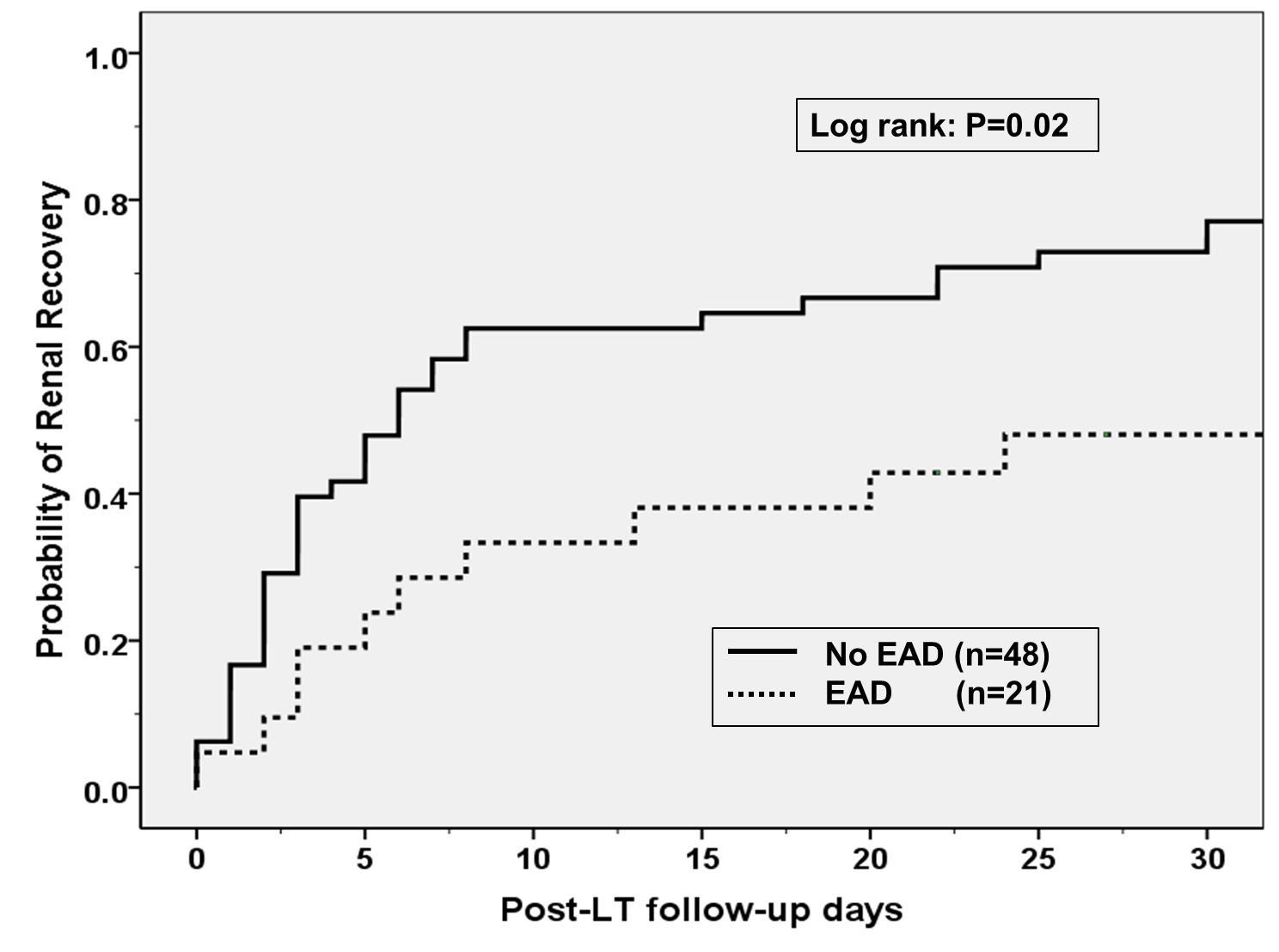 Patients who had EAD and renal non-recovery had the worst 1-, 3 and 5-year patient survival while those without EAD and recovered renal function had the best outcomes (P<0.001)
Patients who had EAD and renal non-recovery had the worst 1-, 3 and 5-year patient survival while those without EAD and recovered renal function had the best outcomes (P<0.001)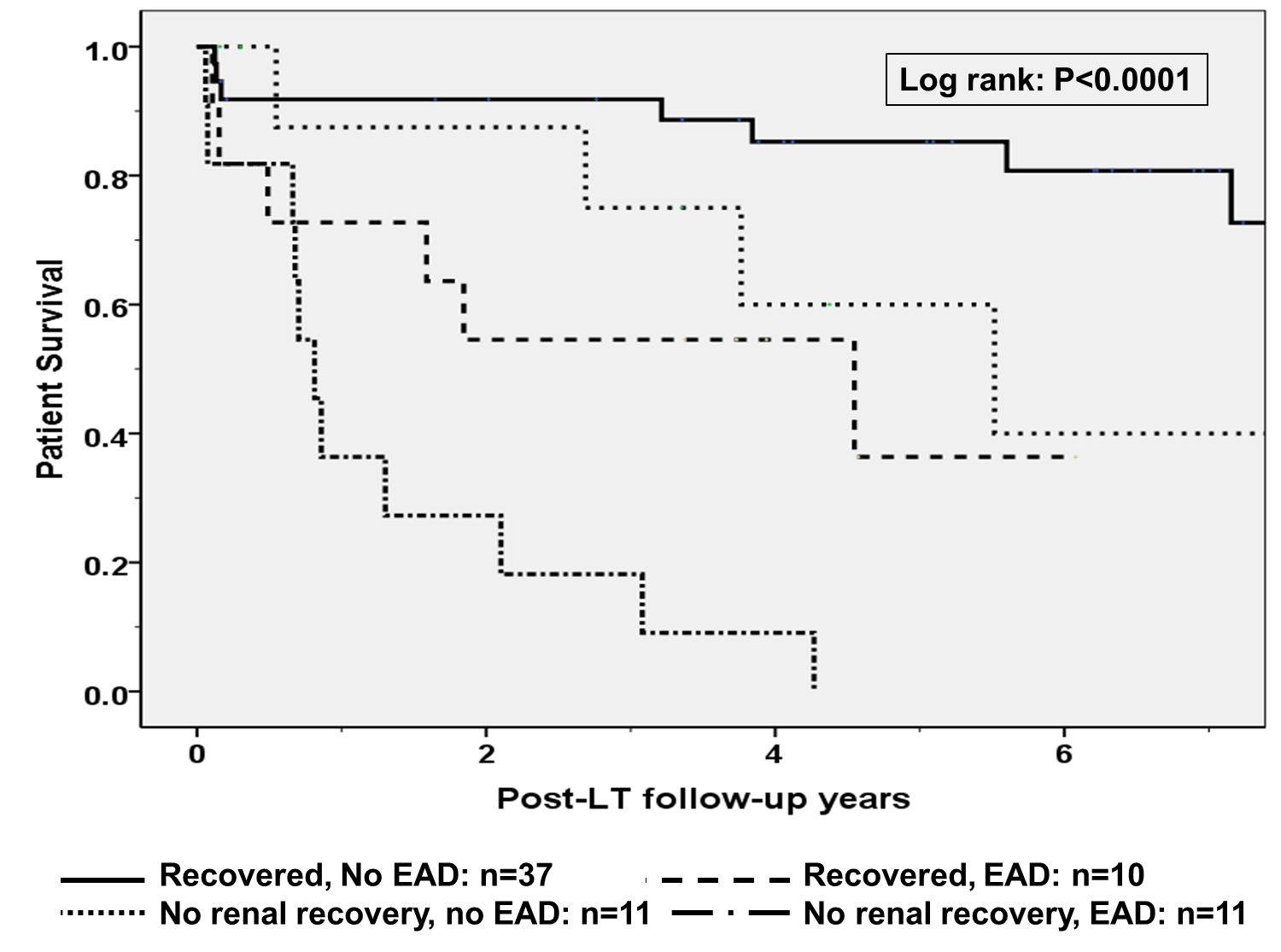
Conclusions: 1) Post-LT EAD was independently associated with lack of renal recovery in LT recipients on RRT for a short duration prior to LT. 2) EAD in the setting of renal non-recovery resulted in the worst long term survival. 3) Measures to prevent EAD should be undertaken in LT recipients on RRT at time of LT.
