MELD Score Predicts Survival in Patients Treated with Transjugular Intrahepatic Portosystemic Shunt after Liver Transplantation
Luis Ibáñez-Samaniego1, María Vega Catalina1, María López1, Manuel González2, Mario Romero1, Aránzazu Caballero1, José Ángel López-Baena3, Diego Rincón1, Mikel Echenagusía2, Rafael Bañares1, Magdalena Salcedo1.
1Liver Unit, Hospital General Universitario Gregorio Marañón, Madrid, Spain; 2Vascular Interventional Radiology Unit, Hospital General Universitario Gregorio Marañón, Madrid, Spain; 3Surgery Department, Hospital General Universitario Gregorio Marañón, Madrid, Spain
Introduction:Transjugular intrahepatic portosystemic shunt (TIPS) is widely used to treat the complications of portal hypertension. Predictors of poor outcome have been described in patients with cirrhosis. However, in the setting of liver transplantation (LT) predictors of mortality are unknown, hence the limited use of TIPS in LT patients who develop portal hypertension. Therefore, the objective of the study was to identify survival predictors in LT patients treated with TIPS.
Patients and Methods: Single-center, retrospective study that analysed demographic, hepatic, hemodynamic, cardiac and technical variables of LT patients treated with TIPS in a tertiary hospital. A Cox regression multivariate model was used to identify predictors of survival. Receiving operator characteristics (ROC) curve identified the most accurate cut-off points and Kaplan-Meier curves and Breslow test were used for the survival analysis. Data is presented as median and interquartilic range or percentage.
Results and Discussion: TIPS was performed in 24 patients (2.1% of 1127 LT patients since 1990): 17 males with a median age of 56 years (48-62). The main indications for TIPS were refractory ascites (75%), portal hypertensive bleeding (20.8%) and portal vein thrombosis (4.2%). The most frequent etiology of LT was hepatitis C related cirrhosis (75%). Time from LT to TIPS creation was 2.3 years (0.7-6.2). TIPS was successfully created in all patients. Immediate complications of the procedure were hepatic encephalopathy (87.5%: grade III-IV: 33%), infections (66.7%) and heart failure (20.8%). Predictors of mortality (table 1) in the univariate model (p<0.10) were age (HR 1.06 [CI95% 0.990-1.145] p=0.092), AST (HR 1.01 [CI95% 1.001-1.019] p=0.027), alkaline phosphatase (HR 1.006 [CI95% 1.001-1.011] p=0.026) and MELD (HR 1.13 [CI95% 0.985-1.297] p=0.081). In the multivariate analysis only MELD remained as an independent predictor of mortality (HR 1.18 [CI95% 1.02-1.365] p=0.026). Area under ROC curve for MELD accuracy to predict mortality was 0.82 being a MELD score of 13 points the best cut-off (sensitivity 86%, specificity 71%). LT patients with a MELD score below 13 points at the time of TIPS creation presented a significantly better two-year survival (80.0% vs 61.9%; p=0.040. Figure 1).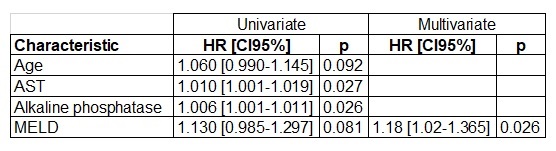
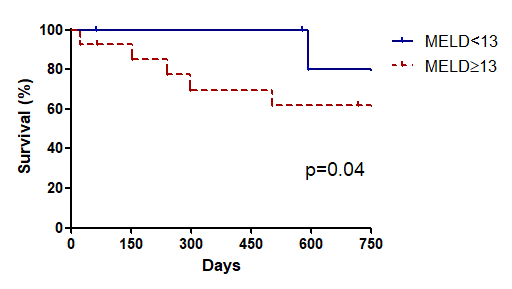
Conclusion: Post-TIPS survival in LT patients is mainly related to liver function (MELD Score) at the time of the procedure. Patients with a MELD score above 13 points have a higher mortality after TIPS creation.
Luis Ibáñez-Samaniego is a recipient of a Rio-Hortega grant (CM14/0023) from Instituto de Salud Carlos III, Spain. .
