Incidence of Mycobacterium Tuberculosis Disease Following Renal Transplant, in a Tertiary Care Hospital in South India
Satish Balan1, Rajalakshmi Arjun2, Ramdas Pisharody1, Praveen Murlidharan1, Sherin Shiny2.
1Nephrology, KIMS Trivandrum , Trivandrum, India; 2Infectious Diseases, KIMS Trivandrum, Trivandrum, India
 Background: India is a high prevalence country for tuberculosis and renal transplant recipients are at higher risk of developing TB (tuberculosis). It is estimated that about 40% of the Indian population is infected with Tubercle bacilli, the vast majority of whom have latent TB rather than TB disease. This study was undertaken to understand the incidence of active TB in this group.
Background: India is a high prevalence country for tuberculosis and renal transplant recipients are at higher risk of developing TB (tuberculosis). It is estimated that about 40% of the Indian population is infected with Tubercle bacilli, the vast majority of whom have latent TB rather than TB disease. This study was undertaken to understand the incidence of active TB in this group.
Methods: Retrospective analysis of 352 patient records who underwent renal transplantation over 12 years, between 2005 to Jan 2017 were included in the study. Routine screening for latent TB with PPD or quantiferon TB test was not done pre-transplant in this centre, as INH mono resistance was reported to be between 8-15% in this part of the country. Post transplant, patients were followed up and treated for active TB. Patients who had renal transplant 10 months or more prior to date of data collection were included, as median time of onset of TB post renal transplantation from previous studies was 9 months. TB was further classified as ‘confirmed’ if AFB smear, AFB culture or molecular test- CB-NAAT is positive, ‘probable’ if in the absence of microbiological test, clinical, radiological or pathological findings favour TB and improve with anti-tuberculous treatment. Incidence of active TB, site of infection, interval between transplant and occurrence of TB, underlying immune-suppression and outcome were studied.
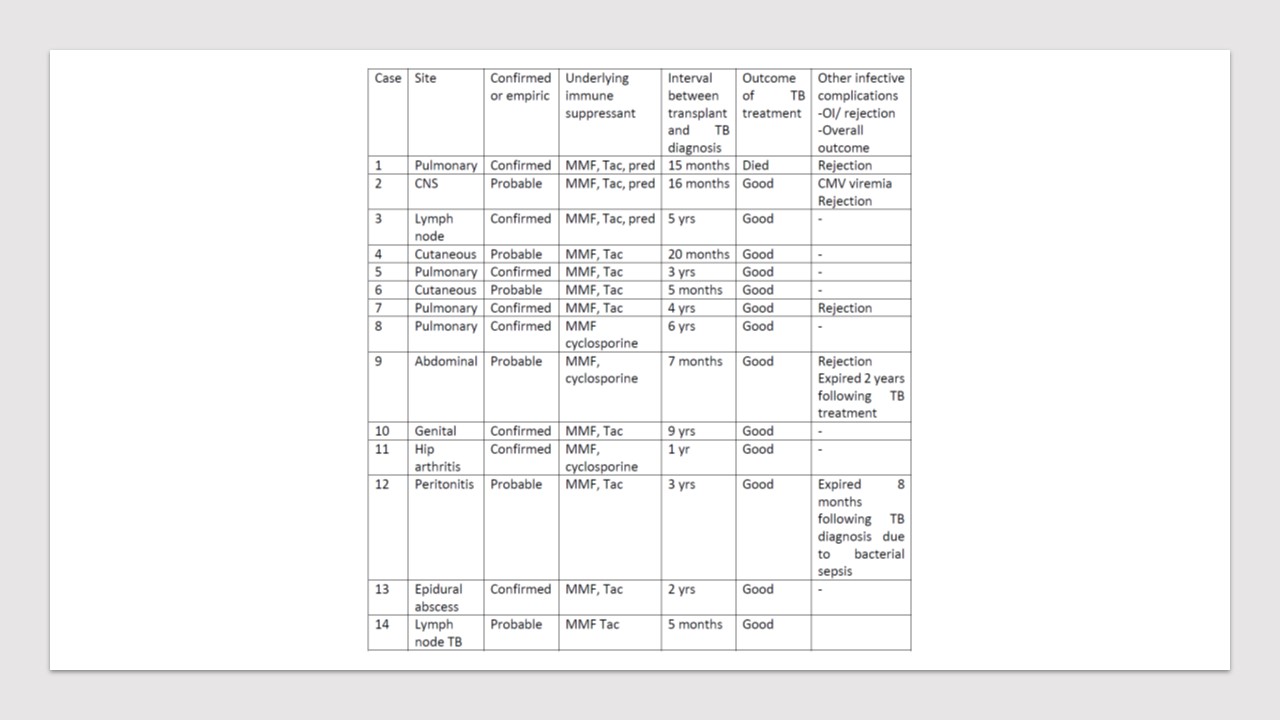
Observations: Among 352 patients 32 patients were lost to follow-up and 27 had died to due an etiology other than TB. 14 had active TB among the 293 patients studied; the incidence being 4.78%. Eight patients had confirmed TB, 6 had probable tuberculosis. Two patients had developed TB within one year of transplantation, the longest time interval was 9 years. Four had pulmonary TB, 10 had extra pulmonary TB. One had rejection 4 years prior to TB diagnosis, 3 had rejection 3 months, 2 and 7 years following TB diagnosis; steroid pulses or intensification of immune suppression were not found to be associated with occurrence of active TB. Combination regime that was commonly used was isoniazid, ethambutol, pyrazinamide and levofloxacin. One patient who was on rifampicin based regime develop rejection following low tacrolimus levels. Rifampicin free regime was used in majority if tacrolimus was used for immune-suppression. Two patients expired 2 years following anti tuberculous treatment due to rejection and other infective complications, rest of them improved and had good outcome.
Results: The incidence of tuberculosis in renal transplant population studied is 4.78% which is lower as compared to other studies from India and Asia. Extra-pulmonary TB occurrence is common and can present in unusual sites like skin. All treated patients had good outcome after TB treatment per se. Understanding the prevalence of latent TB by doing pre-transplant screening in this population will help in determining whether prophylaxis is warranted to prevent development of active TB.
