Renal Allografts from Brain Dead Donors Following Cerebral Gunshot Wounds
Maria Belén Estébanez Montiel 1,2, Mario M Vaca Gallardo 3, Carmen C Gómez Aragón 1, Francisca F Merino Gómez 1, Damiana D Gurria Sanz1, Carlos C Jiménez Martín 3, Eva Mercedes EM Flores Cabeza 2, Alexander A Agrifoglio Rotaeche 2, Eva E Herrero de Lucas 2, Lucía L Cachafeiro Fuciños 2, Pablo P Millán Estañ 2, Manuel Santos MS Sánchez 2, Marcelo M Avilés García 2.
1Transplant Coordination, Hospital Universitario La Paz, Madrid, Spain; 2Intensive Care Unit, Hospital Universitario La Paz, Madrid, Spain; 3Nephrology Department, Hospital Universitario La Paz, Madrid, Spain
Renal allografts from brain dead donors following cerebral gunshot wounds
Introduction: Severe brain injury following cerebral gunshot wounds may expose large amounts of tissue factor to the circulation and develop disseminated intravascular coagulation (DIC). DIC can lead to renal dysfunction.
Objectives: Analyse the validity for transplantation of kidneys harvested from brain dead donors (BDD) following cerebral gunshot wounds and the outcome of the transplanted renal grafts.
Methods: Retrospective descriptive study of renal allografts harvested from BDD following cerebral gunshot wounds, at a single center, between June 1, 2007 and May 31, 2017. Data on donors (patients´ characteristics, blood tests, associated injuries) and recipients (graft survival, rejection) were collected.
Results: We analysed data from six BDD following cerebral gunshot wounds (age 40.3 ± 9.6 years) without any cardiovascular risk factors, except one patient who had hypertension. All patients presented brain death in the first 24 hours of hospital admission. None of them had any associated injuries. One patient suffered a cardiopulmonary arrest (during 20 minutes) prior to ICU admission. One of the patients had elevated creatinine levels in the blood tests when he was admitted to the hospital. But, during the ICU length of stay, up to 50% of the patients presented acute renal failure. Fifty percent of the patients presented compatible or suggestive criteria for DIC. Four kidney grafts were not valid for transplantation because: acute renal failure (two kidney grafts), poor graft perfusion (one case) and complex vascular anomalies (one case). Eight kidney grafts (66.67%) were transplanted. Seven kidney grafts were transplanted in our center. One of them was explanted, in the first 24 hours after transplantation, due to cortical necrosis (pathology report: glomerular and vascular thrombotic microangiopathy lesions). Figure 1. 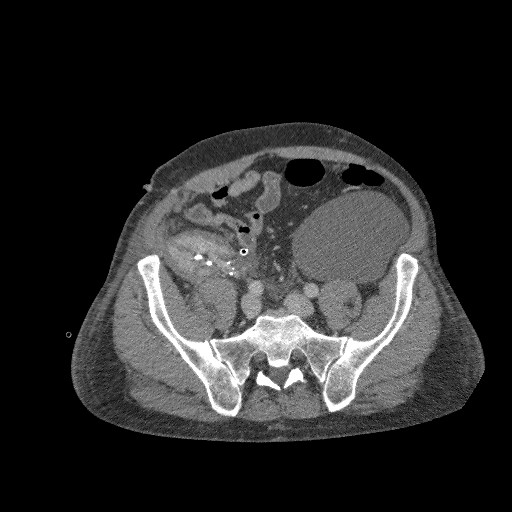 The donor's contralateral kidney was not implanted due to poor perfusion. The pathology report of this kidney was: multiple fibrin trombi in glomerular capillaries and small-vessels (Figure 2).
The donor's contralateral kidney was not implanted due to poor perfusion. The pathology report of this kidney was: multiple fibrin trombi in glomerular capillaries and small-vessels (Figure 2). 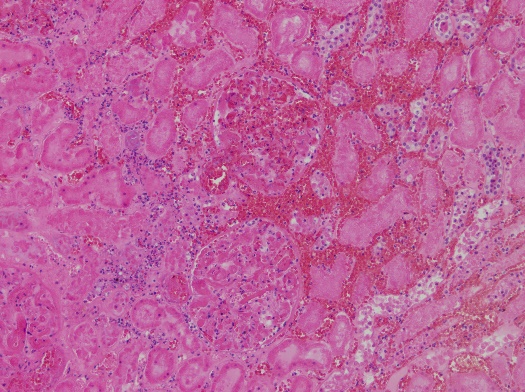 The remaining 6 grafts presented adequate function one year after the transplantation, except in one case which suffered underlying disease recurrence.
The remaining 6 grafts presented adequate function one year after the transplantation, except in one case which suffered underlying disease recurrence.
Conclusion: An accurate evaluation of kidney grafts from BDD following cerebral gunshot wounds is required, because those patients are at risk for DIC and acute renal failure. Almost all transplanted renal allografts from BDD, following cerebral gunshot wounds, had good results in our study. Pre-transplant biopsy and, perhaps, the reduction of ischemia time may be indicated. Further studies with larger simple sizes are needed.
