Utility of Preoperative Non-Contrast Computed Tomography (CT) to Guide Perioperative Management for Renal Transplantation
Evan Werlin1, Joy Walker2, Jonathan Freise1, Anna Mello1, Mehdi Tavakol1, Peter Stock1, Jade Hiramoto2.
1Department of Transplant Surgery, University of California, San Francisco, San Francisco, CA, United States; 2Department of Vascular & Endovascular Surgery, University of California, San Francisco, San Francisco, CA, United States
Background: Peripheral artery disease is highly prevalent among patients with end stage renal disease. Non-contrast CT scans of the abdomen and pelvis (CT A/P) are performed for pre-transplant (tx) evaluation in patients at high risk for cardiovascular events. The purpose of this study is to examine the severity and distribution of common iliac artery (CIA) and external iliac artery (EIA) calcifications and the associations with operative complications and clinical outcomes following renal tx.
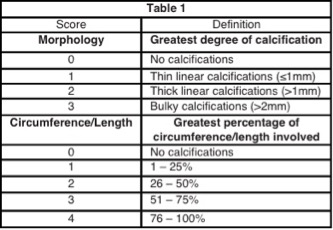
Methods: Retrospective analysis of 202 renal tx recipients between 2/2013-11/2014 who underwent pre-operative CT A/P within 3 years of their surgery. All CT scans were assessed using a previously described scoring system (Table 1).
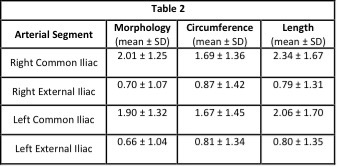
Results: The mean age was 57.2±11.2 years and 132/202 (65%) were men. 189/202 (94%) had hypertension, 124/202 (61%) had diabetes mellitus (DM), and 77/202 (38%) had coronary artery disease (CAD). There was no significant difference in calcification scores between sides (Table 2). In a regression analysis, previous cerebrovascular accident (CVA) (OR 5.43, p=0.03), CAD (OR 3.56, p<0.001), history of smoking (OR 2.08, p=0.02), DM (OR 2.23, p=0.01), and older age (OR 1.10, p<0.001) were significantly associated with moderate/severe CIA plaque (morphology score ≥ 2). One patient could not undergo tx due to severe, diffuse calcifications. 7 patients required arterial reconstruction during renal tx, all of whom had tx to the right EIA. Patients with moderate/severe right EIA plaque were more likely to require arterial reconstruction compared to those with none/mild plaque (4/34 [11.7%] v. 3/130 [2.3%]; p=0.03). There were 58 cases of delayed graft function (DGF), 51 of which occurred in transplants to the right EIA. In these cases, DGF was significantly associated with moderate/severe right EIA plaque (OR 2.82, p=0.009). Post-operative cardiac events occurred in 17/201 (8.5%) patients. In a multivariable logistic regression model, history of CAD (OR 3.79, p=0.03), congestive heart failure (OR 5.54, p=0.009), and severe CIA plaque (morphology score=3) (OR 4.98, p=0.04) were significantly associated with post-operative cardiac complications. 21 patients died during a mean follow-up of 1153 ± 1784 days. In a multivariable model, DM (p=0.05) and previous CVA (p=0.02) were significantly associated with increased risk of death.
Conclusions: Local calcified plaque of the recipient iliac artery is associated with increased operative complexity and higher rates of DGF. Plaque burden in the CIA is associated with both patient demographic factors and post-operative cardiac events, and is likely indicative of a greater severity of systemic atherosclerotic disease. Routine pre-tx CT scans in high risk patients may guide operative strategy and facilitate perioperative management to improve clinical outcomes. |
Research reported in this publication was supported in part by an NIAID T32 training grant from the National Institutes of Health under an award to the University of California, San Francisco (T32AI125222). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
