Standard induction immunosuppression interferes with the role of vascularized bone marrow in vascularized composite allograft protection
Nicole Shockcor1, Bryan Buckingham1, Wessam Hassanein1, Arthur J Nam1, Stephen T Bartlett1, Rolf N Barth1.
1Department of Surgery, University of Maryland School of Medicine, Baltimore, MD, United States
Introduction:Clinical induction therapies have been demonstrated to interfere with the development of immunologic tolerance in experimental models. Vascularized bone marrow (VBM) has been demonstrated to provide immunologic protection to vascularized composite allografts (VCA). We utilized a non-human primate (NHP) model of facial transplantation to investigate the effects of recipient T cell depletion and steroid therapy on VBM-mediated graft protection.
Materials and Methods: We utilized a well-established model of heterotopic facial subunit VCA in a NHP model. Recipients (N=3) were administered 50 mg/kg of anti-thymocyte globulin (ATGAM) on Day -2, -1, and 0 and transplanted Day 0. Steroids were administered with an initial 20 mg/kg dose and tapered over 21 days and maintained on tacrolimus (Tac) and mycophenylate mofetil (MMF). Chimerism was determined using flow cytometry from peripheral blood samples and final tissues. Comparison was made to historical cohorts, VCA + VBM (n=4) and VCA (no VBM, n=3) treated with Tac/MMF.
Results and Discussion: Mean survival in the ATGAM with steroid taper group was 28.3 ±8.02 days, as compared to VCA + VBM group 348.2±85.9 days, and VCA (no VBM) 24.7±16.6 days (p=0.008). 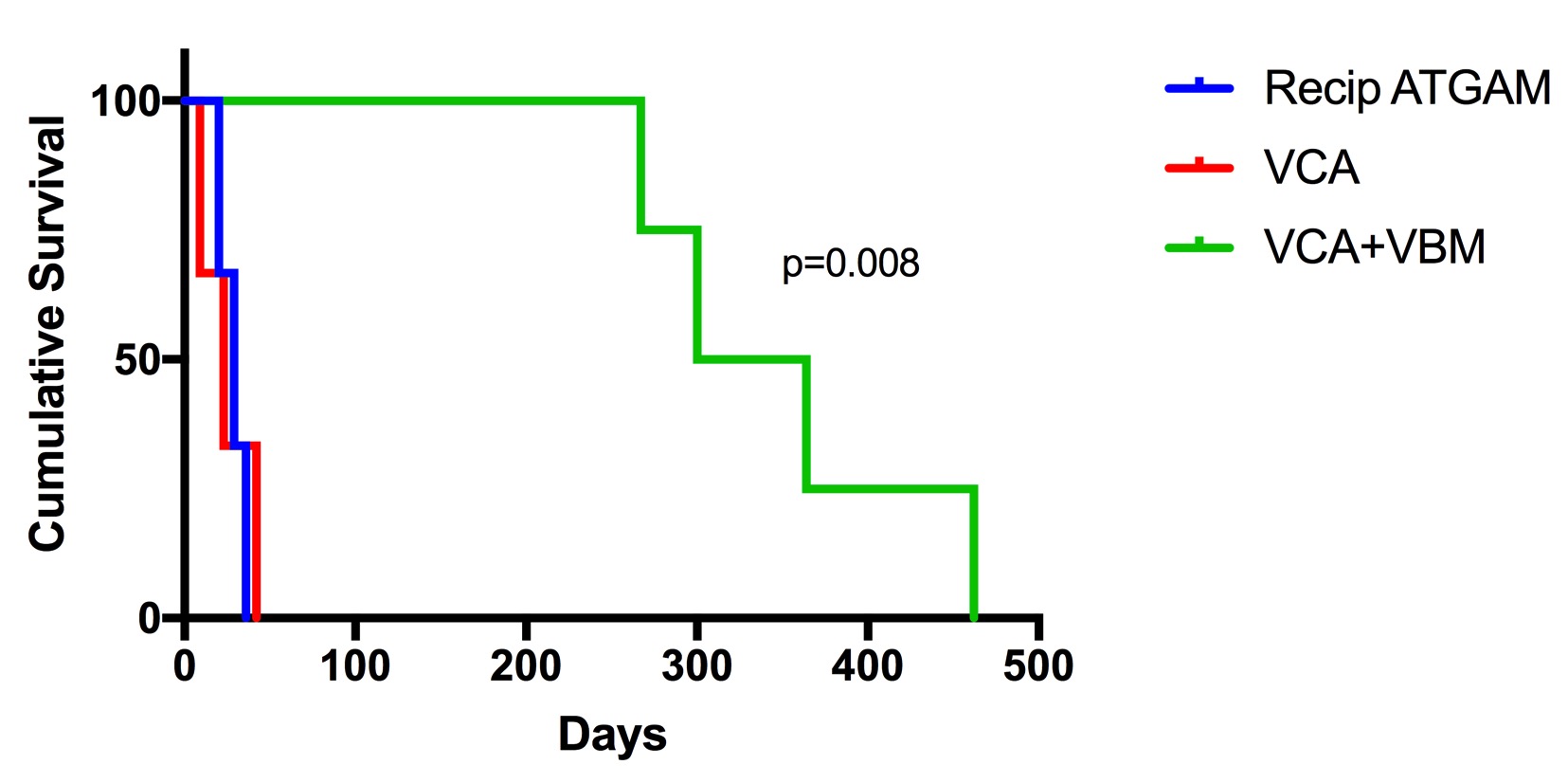 NHP receiving induction therapies developed early Banff 4 rejection, as well as histopathologic evidence of thrombophlebitis and muscle necrosis. In contrast to the VCA + VBM group, chimerism was undetected in peripheral blood and graft bone marrow was nearly acellular, with an average of 91.5%±2.4 (range 89.8-93.2%) of the lymphocytes present recipient in origin (n=2). Also in contrast to VCA + VBM but comparable to VCA (no VBM), the development of IgM and IgG donor specific antibodies was noted in the ATGAM with steroid taper group, with a mean of 357.5 and 180.5 MFI respectively.
NHP receiving induction therapies developed early Banff 4 rejection, as well as histopathologic evidence of thrombophlebitis and muscle necrosis. In contrast to the VCA + VBM group, chimerism was undetected in peripheral blood and graft bone marrow was nearly acellular, with an average of 91.5%±2.4 (range 89.8-93.2%) of the lymphocytes present recipient in origin (n=2). Also in contrast to VCA + VBM but comparable to VCA (no VBM), the development of IgM and IgG donor specific antibodies was noted in the ATGAM with steroid taper group, with a mean of 357.5 and 180.5 MFI respectively.
Conclusion: Presumptive VBM cell populations that regulate immune responses are susceptible to T cell depleting and steroid therapies. The observed interference of standard induction therapies on the protective value of VBM highlights relationships between pharmacologic and biologic mechanisms of VCA graft protection.
Astellas Pharma US, Inc.. Henry Jackson Foundation, Department of Defense Award # W81XWH-13-2-0056.
