Deceased Organ Donor Screening for Trypanosoma Cruzi in the UK - A Strategy in a Non-Endemic Country
Ines Ushiro-Lumb1,2, Mhairi Webster1, Alan Kitchen1.
1Microbiology Services, National Health Service Blood and Transplant, London, United Kingdom; 2National Infection Service, Public Health England, London, United Kingdom
Background: In the UK, the Advisory Committee on Microbiological Safety of Blood, Tissues, Organs and Cells (SaBTO) recommends discretionary T. cruzi antibody screening of donors with identified risk factors for American trypanosomiasis. Centralised T. cruzi antibody screening of deceased organ donors was introduced by the single organ procurement organisation, NHS Blood and Transplant (NHSBT), in 2014. In England, blood donors have been tested on a discretionary basis since 2009, with a current incidence of 0%.
Aims: To describe the strategy for assessment of donor risks for Chagas disease in a non-endemic country and report results of donor screening implementation.
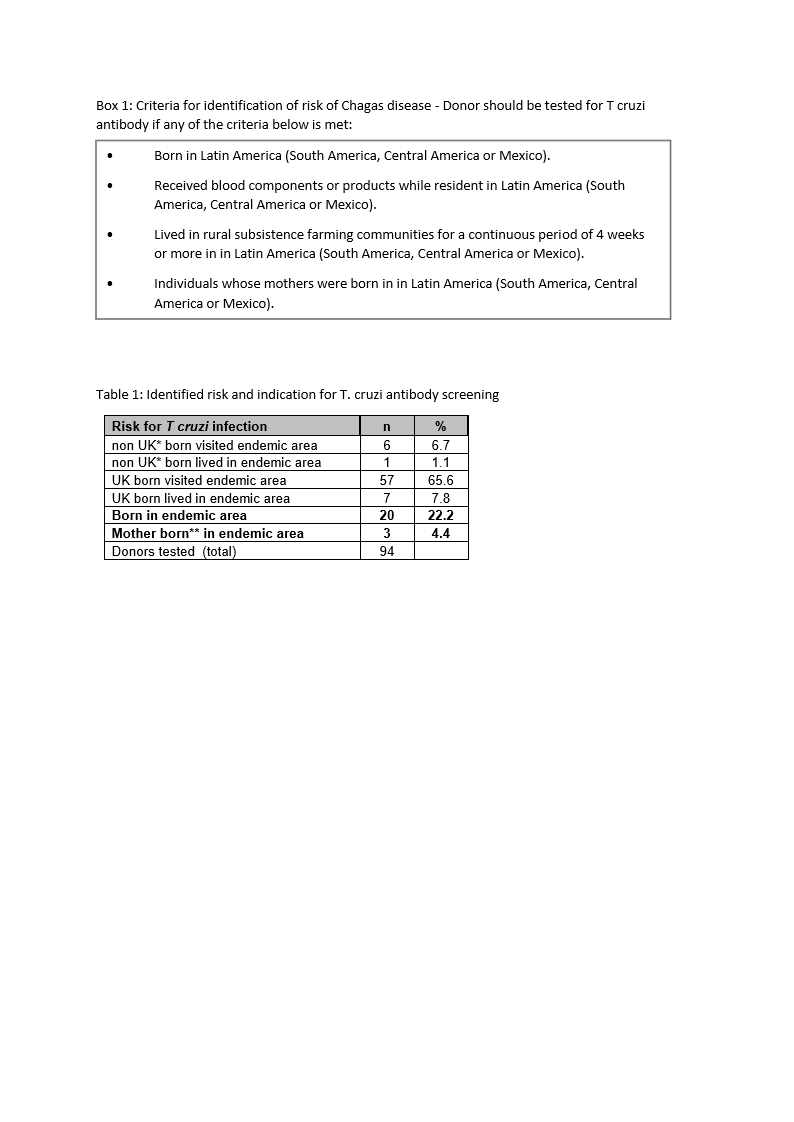
Methods: Indication for testing is identified through interview with next of kin (NoK) and medical history obtained from the donor’s general practitioner. T. cruzi antibody screening should be undertaken in donors that meet any of the criteria shown in box 1. Requests submitted for T. cruzi Ab from deceased organ donors in England, N Ireland and Wales between July 2014 - July 2017 were reviewed for data collection. Bio kit Chagas Antibody® initially and then Abbott Architect Chagas ® assays were used as per manufacturer’s instructions.
Results: Risk of exposure to T. cruzi was identified in approximately 94/5100 consented deceased organ donors (1.84%), a higher proportion than that identified amongst blood donors in England (0.07%). Indications for testing are summarized in table 1. The commonest indication was travel to potentially endemic areas (72.3%), whilst residency in endemic areas accounts for 35.5% of requests. There were no seropositive results.
Discussion: Identification of risk is based largely on demographic and travel information obtained from the NoK at the time of donation, which is less precise when compared to live donor history, resulting in a lower specificity of selection. True risk of infection is associated with distinctive factors and prolonged exposure in rural, endemic or hyper endemic areas; donor or family history of conditions compatible with Chagas disease may also be present and must be noted. The risk of T. cruzi in our donor population remains very low, reflecting the composition of migrant populations in the UK. The commonest indication for testing is travel to endemic areas, whereas the higher risk indicators are seen in 36% of those tested. In the setting of a non-endemic area, emphasis has been on detailed donor history, with immediate post-donation screening as prompt identification of infected donors in the immediate post-transplant period will still inform modified recipient management and allow mitigation of morbidity through appropriate monitoring and pre-emptive treatment, as required.