Low Utilization Rate of Hearts Designated as PHS Increased Risk and Presumed Infected
Charles Wright1, Hesham Omar3, Maya Guglin2.
1LifeLink of Florida, Tampa, FL, United States; 2University of Kentucky, Lexington , KY, United States; 3Mercy Medical Center, Clinton, IA, United States
Introduction: Disease transmission is always a concern in transplantation. The USPHS has published a guidance document to determine the potential risk of transmission of HIV, HCV and HBV through transplantation. The designation of PHS Increased Risk (IR) is assigned to donors with behaviors shown to increase the risk of HIV, HCV and HBV and the designation of PHS Presumed Infected (PI) is given to donors with testing indicating infection with HIV, HCV or HBV. It has been suggested in the literature that these designations have resulted in the non-utilization of suitable organs. In this observational study we explore the impact of PHS IR and PHS PI on the utilization of normal donor hearts.
Materials and Methods: During this prospective observational study at a single organ procurement organization in the United States (LifeLink of Florida) for one year (10/14 – 10/15) all deceased organ donors < 60 years old with authorization for research were enrolled in the study. Data on medical history, ECHO and when indicated coronary angiography were collected. Hearts were designated as normal if there was no known heart disease, ECHO showed the LVEF > 50% with no LVH and no coronary artery disease on angiography when performed.
Results: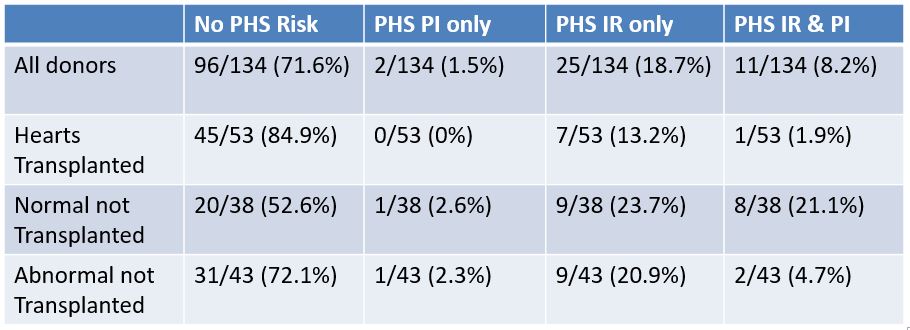 Of the 134 hearts evaluated, 53 (39.5%) were transplanted and 38 (28%) were PHS IR, PI or both. Only 8 (15%) transplants were PHS IR or PI. Thirty-eight hearts were normal by all clinical evidence and were not accepted for transplantation, of this group 18 (47%) had PHS risk factors. Transplanted hearts were more likely to have no PHS risk factors than normal non-transplanted hearts (84.9% vs. 52.6% P=0.001). Using Fisher exact due to small n, normal non-transplanted hearts were more likely to have PHS risk factors compared to transplanted hearts (21.1% vs. 1.19%, P=0.004). All donors had abdominal organs transplanted and no transmission of HIV, HCV or HBV was observed.
Of the 134 hearts evaluated, 53 (39.5%) were transplanted and 38 (28%) were PHS IR, PI or both. Only 8 (15%) transplants were PHS IR or PI. Thirty-eight hearts were normal by all clinical evidence and were not accepted for transplantation, of this group 18 (47%) had PHS risk factors. Transplanted hearts were more likely to have no PHS risk factors than normal non-transplanted hearts (84.9% vs. 52.6% P=0.001). Using Fisher exact due to small n, normal non-transplanted hearts were more likely to have PHS risk factors compared to transplanted hearts (21.1% vs. 1.19%, P=0.004). All donors had abdominal organs transplanted and no transmission of HIV, HCV or HBV was observed.
Discussion: Our data indicates that the designation PHS IR and PHS PI appears to decrease the utilization of hearts otherwise suitable for transplantation. Volk et al showed that kidneys designated as PHS IR were less likely to be transplanted. UNOS has recently published a guidance document for transplant centers which includes data showing very low risk of transmission of HIV, HCV and HBV with current testing platforms. The risk of transmission of HIV from a donor with a history of current IVDA and negative NAT testing is 4.9 / 10,000 donors. Studies are currently under way intentionally transplanting HCV positive kidneys into HCV negative recipients with early treatment of HCV with excellent early results. In 2015, 405 patients died waiting for a heart transplant in the United States.
Conclusion: To avoid deaths while waiting for heart transplantation, heart transplant programs need to consider the actual risk of utilization of PHS IR hearts and consider more aggressive utilization of PHS IR and PI hearts.
LifeLink Legacy Fund.
