Immune Profiling in Highly Sensitized Kidney Transplant Recipients
Sarita Negi1, Alissa Rutman1, Steven Paraskevas1, Jean Tchervenkov1.
1Department of Surgery, McGill University, Montreal, QC, Canada
Introduction: Recipient sensitization to human leukocyte antigens (HLA) is a critical problem in clinical transplantation. Highly sensitized patients (HSP) express non-self HLA antibodies and remain on the transplant waitlist due to higher probability of positive cross match to potential donors. They also have poor graft survival due to higher incidences of acute or chronic rejection as compared to non-sensitized patients (NSP). Sensitized patients receiving extended criteria donor (ECD) kidneys show decreased graft function but increased allograft injury of one year. They also have poor allograft survival of 7 years and antibody mediated rejection (ABMR) is main cause of graft loss. Inflammatory cytokines like (IL4, IL5, IL6, IL17) secreted by T-helper cells (Th) induce B-cell proliferation and differentiation. We hypothesize that Th and B-cells play key role in allosensitization of HSP leading to graft loss and therefore sought to compare immune responses between HSP and NSP.
Materials and Methods: Peripheral blood mononuclear cells (PBMC) were isolated from HSP(n=16) and NSP(n=13). PBMC were cultured overnight and stimulated with PMA/ionomycin/Brefeldein for 6 hrs. Intracellular cytokine (IFNg, IL4, IL6, IL17, TNF) expression in CD4, CD8 and CD19 cells was analyzed by Flow Cytometry. One way multiple leukocyte reactions (MLR) were performed to measure antigen-specific stimulation. Recipients PBMC were primed with irradiated donor antigen-presenting cells (APC) carrying unacceptable HLA antigens (U-dAPC) or a matched donor APC (M-dAPC) for 6 days. In some cases, PMA was added for last 6 hours of culture.
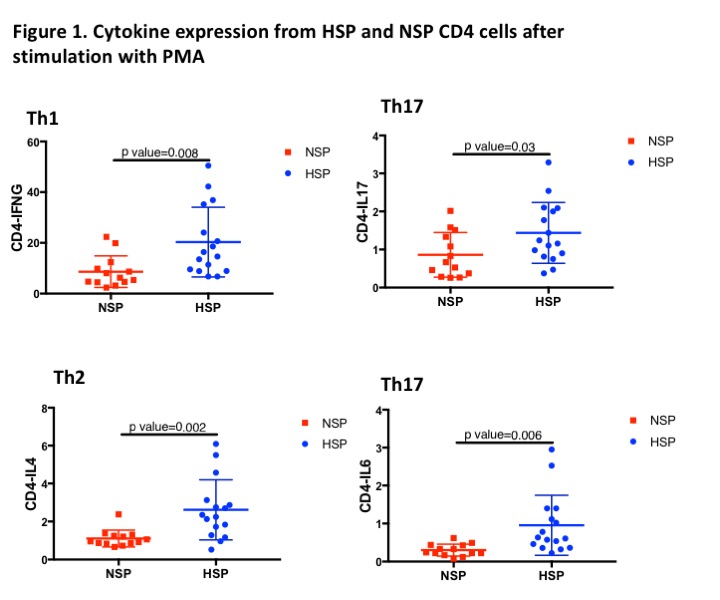
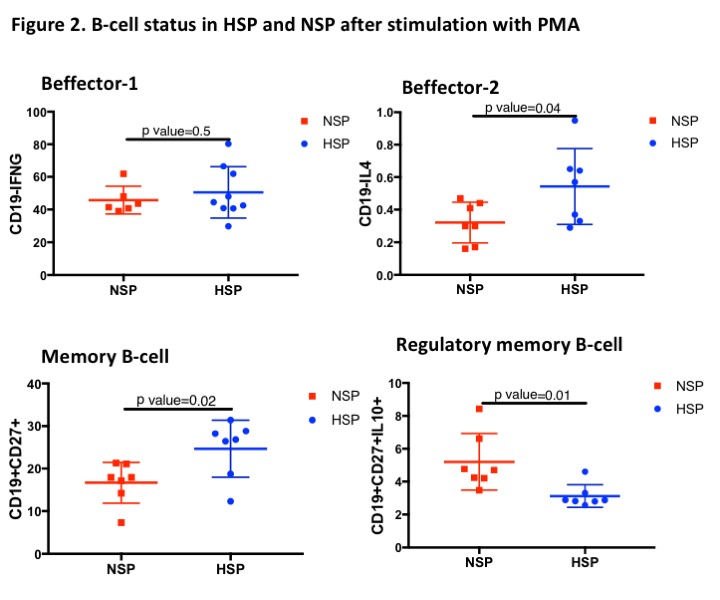
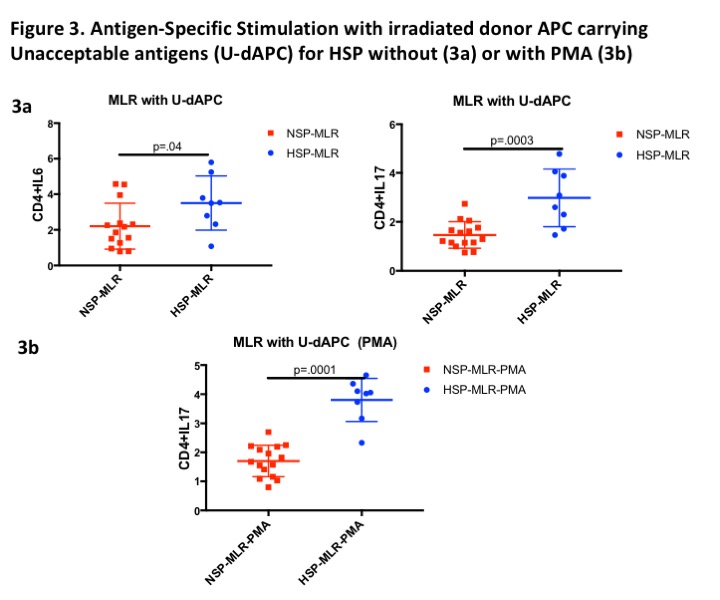
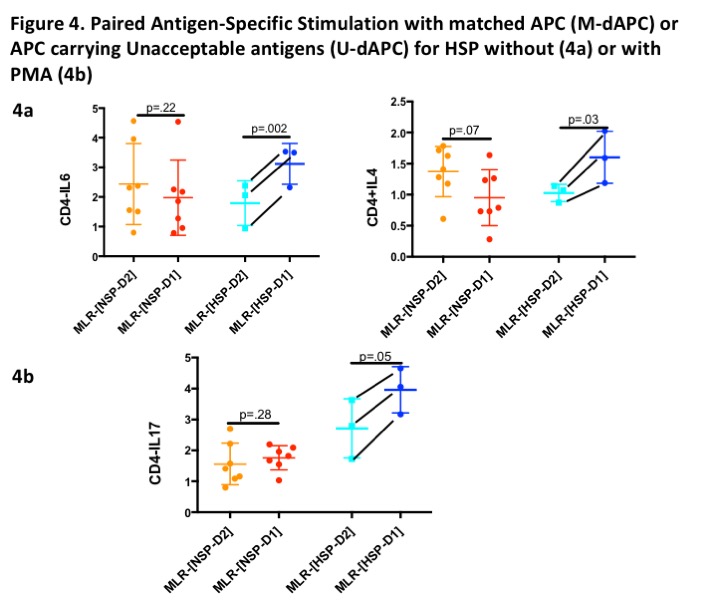
Results and Discussion: Non-specific stimulation with PMA significantly increased (IFNg+, IL4+, IL6+, IL17+ TNF+) expressing CD4 cells and (IFNg+, IL4+) expressing CD19 cells in HSP. These results indicate a higher degree of T-cell and B-cell mediated immune activity in HSP. In HSP, CD19+CD27+ memory B-cells were increased but memory Breg (CD19+CD27+IL-10+) subset was decreased indicating impaired activation of memory Breg. Antigen-specific MLR with U-dAPC induced higher percentage of CD4+IL6 and CD4+IL17 cells in HSP only. CD4+IL17+ cells in HSP remain significantly higher with PMA. These results indicate that IL6 and IL17 may have a role in B-cell activation in HSP.
Unmatched donor significantly increased CD4+IL4 and CD4+IL6 cells without PMA and, induced CD4+IL17 cells with PMA in HSP only suggesting that IL4, IL6 and IL17 may mediate antigen-specific immune response in HSP. Conclusions: Results suggest that HSP may have potent Th1, Th2 and Th17 mediated immune response as compared to NSP. Th1, Th2 and Th17 are known to play role in graft rejection and IL6/TGFb signaling promotes Th17 differentiation. Therefore, IL4, IL6 and IL17 may be playing crucial role in ABMR and graft loss in HSP. The blockage of IL6 and IL17 signaling pathways could be an attractive approach to reduce the risk of post-transplantation rejection for HSP.