Prevalence of Anal Cytological Abnormalities and Human Papilloma Virus: A Cohort Study in Kidney Transplant Recipients
Brenda Rosales1, Julian Langton-Lockton2, Jennifer Roberts 3, Sepehr Tabrizi4, Andrew Grulich5, Richard Hillman6, Angela C Webster1,7.
1Sydney School of Public Health, University of Sydney, Sydney, Australia; 2West Sydney Sexual Health Centre, Western Sydney Local Health District, Sydney, Australia; 3Douglas Hanly Moir Pathology, Sydney, Australia; 4Molecular Microbiology, Murdoch Children's Research Institute, Melbourne, Australia; 5The Kirby Institute, Sydney, Australia; 6St Vincent’s Hospital, Sydney, Australia; 7Renal Medicine and Transplantation, Westmead Hospital, Sydney, Australia
Introduction: Transplant recipients have twelve times the risk of anal cancer as the general population in Australia and New Zealand. High risk human papilloma virus (hrHPV) genotypes cause 80-90% of anal cancers. High grade squamous intraepithelial lesions (HSIL) are the precursor of anal cancer. Anal swab testing could be used as a screening tool. We sought to determine the presence of HPV and anal cytological abnormalities in kidney transplant recipients, and assess the feasibility of an anal cancer screening intervention.
Materials and Methods: Kidney transplant recipients, over 18 years old, attending Westmead Hospital, Sydney, were prospectively recruited from 2014-2017, and underwent anal swabbing. Anal liquid-based cytology samples were subjected to cytological examination and HPV genotyping.
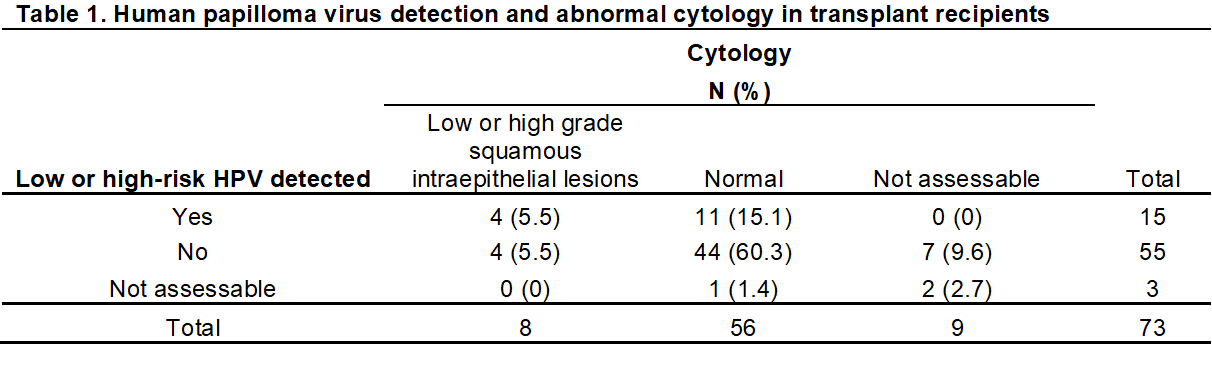
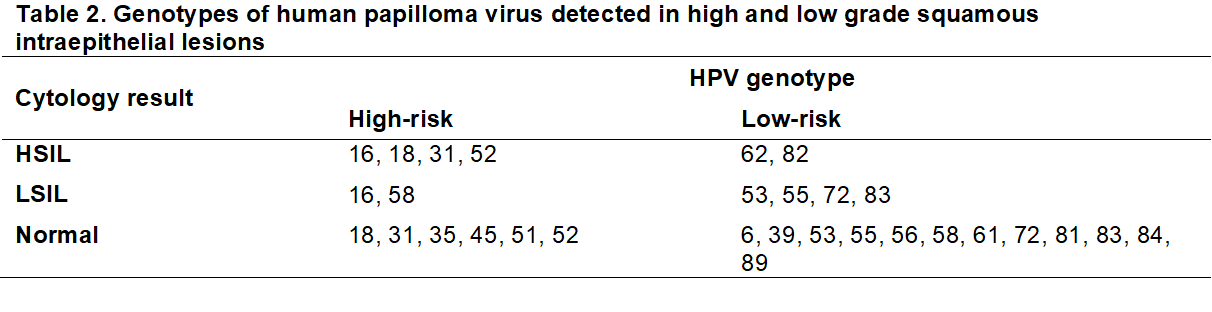
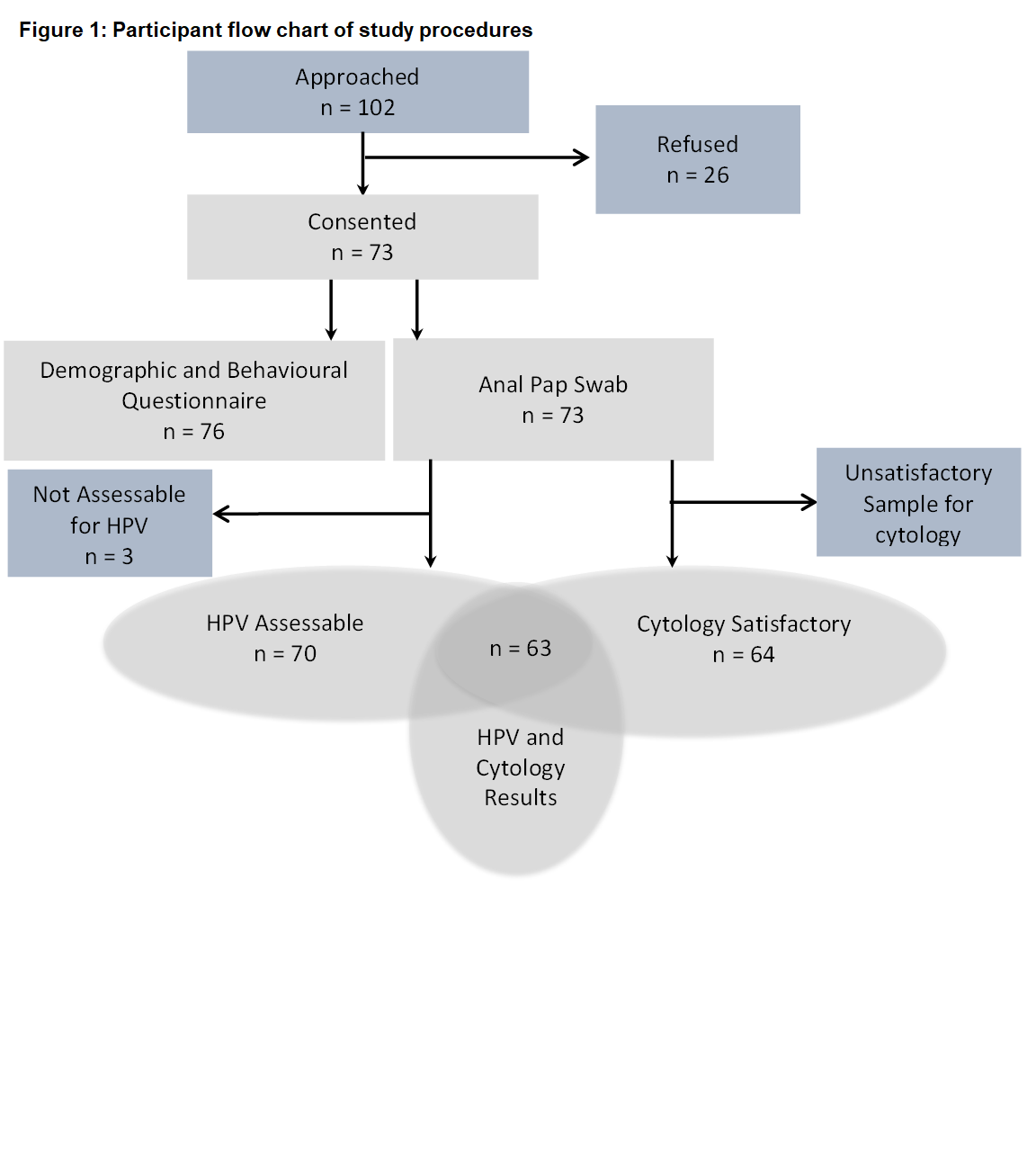
Results and Discussion: To date, of 102 eligible participants approached, 73 (72%) consented to join the study and completed testing (Figure 1). The mean age was 47 (median=47, range 20-76 years). 64 (88%) had technically satisfactory cellularity. Of these, 8 (12.5%) were abnormal; 6 (9.4%) showed Low grade Squamous Intraepithelial Lesion (LSIL); 2 (3.1%) HSIL and 56 were negative. Of 73 specimens HPV genotyped, 70 (96%) were assessable. HPV was detected in 15 (20.5%) participants; 9 (12.3%) participants had one or more high-risk genotypes detected. The proportion of HPV positive participants with abnormal cytology was over three times that of those with no HPV; 4 (27%) of 15 HPV positive participants had abnormal cytology, compared to 4 (7%) of 48 with no HPV. However, there was no evidence of an association between any HPV detection (low or high-risk) and abnormal anal cytology (OR 2.75, 95%CI 0.82-11.84); p=0.12). Both participants with cytological HSIL were confirmed to have histological HSIL on high resolution anoscopy. One participant had HPV types 16, 18 and 62, the other HPV types 31, 52 and 82.
Conclusions: Transplant recipients were generally willing to consent to the study procedures, including anal swabbing. The prevalence of abnormal cytology was 12.5% and high risk HPV genotypes 12.3%. Anal swabbing was able to identify individuals at increased risk of anal cancer for future close monitoring. (Australian New Zealand Clinical Trials Registry (ANZCTR); ACTRN12616001507471)
Sydney Medical School Foundation.
